Skin conditions could indicate risk of complication after surgery for retinal detachment
Patients with a history of cutaneous keloids, hypertrophic scarring or fibrosis are more likely to have proliferative vitreoretinopathy (PVR) following surgery to repair a detached retina. A recent Cleveland Clinic study is among the first to show this association.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
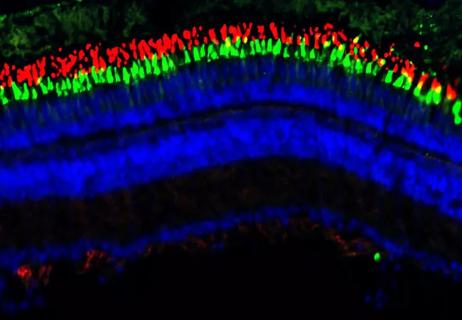
PVR is a rare complication of abnormal scarring of the retina following either chronic retinal detachment or surgery. It occurs in 5%-11% of retinal detachment cases. Risk factors include smoking, trauma, large retinal tears, previous surgery and chronicity.
“Often, when ophthalmologists describe PVR to patients, we compare it to cutaneous scarring after a cut or other skin damage,” says Danny A. Mammo, MD, a vitreoretinal disease and uveitis specialist at Cleveland Clinic Cole Eye Institute. “However, to date, there have been no studies that prove a correlation between being prone to cutaneous scarring and risk of retinal scarring.”
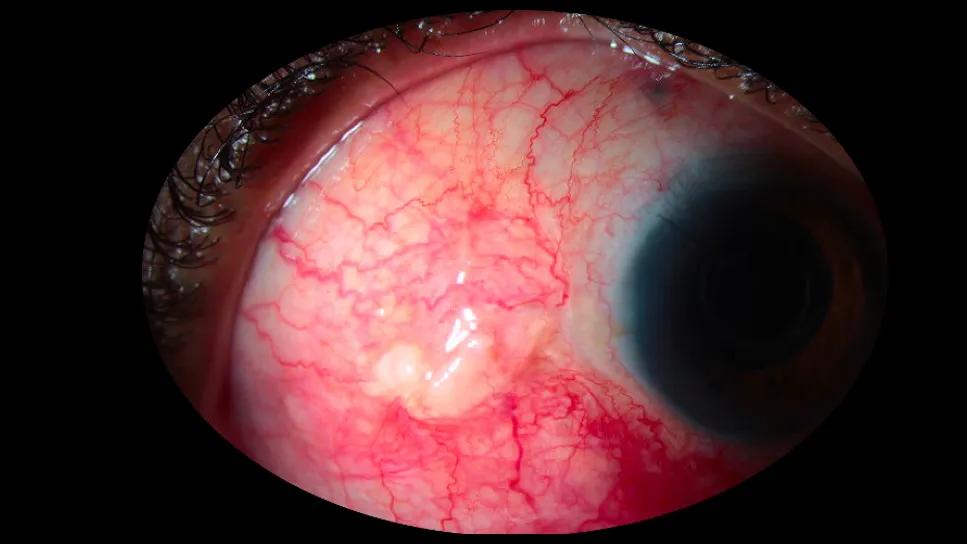
One of Dr. Mammo’s patients treated for retinal detachment had numerous cutaneous keloids from prior injuries. Following the surgery to repair his retinal detachment, the patient developed conjunctival keloids as well as PVR. That case inspired Dr. Mammo to explore the association.
“The availability of a large database made the study possible,” Dr. Mammo says. “Before big data, researchers could evaluate only a limited number of patients, often from their own institution. Now we have access to the medical records of tens of thousands of patients, which can provide a clearer picture.”
The retrospective study, recently published in Ophthalmology, included more than 25,000 patients who had a noncomplex retinal detachment repair with pars plana vitrectomy between 2003 and 2023. According to International Classification of Diseases, 10th Revision (ICD-10) codes in the research database, about 1,100 of the patients had cutaneous keloids, hypertrophic scarring or fibrosis. Of that group, 10.1% had PVR within six months of surgery, compared with only 3.4% of patients without cutaneous keloids, scarring or fibrosis.
Advertisement
In addition, 8.3% of patients with cutaneous keloids, scarring or fibrosis had a complex retinal detachment repair within six months of the first surgery, compared with 5.4% of other patients.
“The presence of PVR can cause the retina to detach again, requiring additional surgery,” explains Dr. Mammo, the study’s first author. “By definition, that second surgery is for ‘complex’ retinal detachment. That’s why we looked at complex repairs as well. They could imply that PVR was more prevalent than the diagnostic codes originally indicated.”
The research team then studied a larger group of patients, adding in those who had retinal detachment repair with two less common procedures: pneumatic retinopexy and primary scleral buckle. Of those 34,000 patients, nearly 1,500 had cutaneous keloids, scarring or fibrosis, 9% of whom had PVR within six months of surgery and 8% of whom needed subsequent complex repair. Only 4.2% of the patients without cutaneous keloids, scarring or fibrosis had PVR within six months, and 6.4% needed complex repair.
“These results indicate that a dermatologic history of keloids, hypertrophic scarring or fibrosis could be considered a risk factor for PVR after surgery to repair a retinal detachment,” Dr. Mammo says.
Intravitreal methotrexate may help reduce the risk of PVR after surgery. Additional therapies are being studied. Better identifying patients at increased risk of PVR will allow physicians to use therapies more efficiently.
“Incorporating therapies to prevent PVR is a newer development,” Dr. Mammo says. “We wouldn’t use therapies like methotrexate in every patient — just those at higher risk of PVR. Patients with a history of cutaneous keloids, hypertrophic scarring or fibrosis may potentially be included in that group.”
Advertisement
Advertisement

The advanced stage of diabetic retinopathy is among the most challenging for retinal surgeons

Watch for sudden unilateral vision loss without pain

Prematurity is linked with poorer outcomes of retinal surgery in adulthood

A primer on sustained release options

New study counters earlier findings linking drugs with eye disease

How to screen for and manage treatment-triggered uveitis
Researchers to study retinal regeneration in zebrafish with new grant from National Eye Institute

Leukocoria is the most common symptom of this rare childhood eye cancer