Study offers guidance on an increasingly common presentation

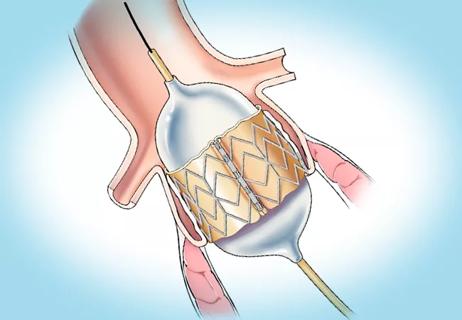
Cardiac operations after transcatheter aortic valve replacement (TAVR) are increasing in frequency, and the time between TAVR and subsequent cardiac surgery is shrinking. So finds a retrospective study out of Cleveland Clinic published in the Annals of Thoracic Surgery (2022;114:52-60).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Noting an increase in post-TAVR patients referred for heart surgery, Cleveland Clinic surgeons sought to determine the indications, frequency and outcomes of these operations performed at their institution. The study represents the largest investigation from a single center with multiple surgeons addressing this patient population.
“We found that most cases were complex operations with a high predicted mortality rate,” says Cleveland Clinic cardiothoracic surgeon and first author James Yun, MD, PhD. “This brings to light the importance of considering potential future cardiac surgery when helping patients choose the best approach for initial aortic valve replacement (AVR). It’s particularly important in younger patients with low or intermediate surgical risk who have a longer life expectancy. In these patients, accounting for future cardiac operations after TAVR, especially when the patient’s cardiac pathology is not fully addressed by TAVR alone, is imperative.”
From January 2012 to July 2020, 59 patients underwent post-TAVR cardiac surgery at Cleveland Clinic; nearly two-thirds had undergone TAVR at another institution.
The frequency of post-TAVR surgery increased over time, with fewer than 10 such operations performed annually through 2018, in contrast to 18 performed in 2019 and nine in the first 6 months of 2020. The interval between TAVR and cardiac surgery decreased from 7 years to less than 1 year over the course of the study period.
Median patient age was 70 years, and 71% were men. Forty patients (68%) underwent complex operations without a calculable Society of Thoracic Surgeons predicted risk of mortality (STS PROM); for the remainder, the median STS PROM was 5.5%. The TAVR valve was explanted in 46 cases (78%); only five (8.5%) were isolated surgical aortic valve replacements (SAVR), and 36 (61%) were redo sternotomies because of a history of prior open cardiac surgery.
Advertisement
Operative mortality was 8.5% — notably half of the 17% mortality reported in a 2020 analysis of surgical reoperation after TAVR using 2011-2015 data from the STS Adult Cardiac Surgery Database. Rates of other complications included the following:
“These surgeries are complex. For the best results, an experienced surgical team needs to intervene at the right time,” says Dr. Yun. “When patients are properly selected, reasonable outcomes are feasible.”
“Because of the scope and complexity of such procedures, and because some patients have a heavy burden of comorbidities, the risk of morbidity and mortality is significant and higher than for isolated AVR,” adds study co-author Faisal Bakaeen, MD, another Cleveland Clinic cardiothoracic surgeon. “That is why experience in cardiac reconstructive surgery and reoperations is a must for surgeons contemplating operating on patients who have undergone TAVR.”
The leading indications for post-TAVR cardiac surgery were TAVR valve stenosis or regurgitation (58%), paravalvular leak (24%) and endocarditis (17%). In cases where the TAVR valve was not explanted, mitral regurgitation was the primary indication for surgery.
“Patients with significant mitral or coronary artery disease that was not addressed at the time of TAVR come in needing a valve or bypass in open surgery,” notes Dr. Bakaeen. “When the issue is TAVR valve malfunction, it sometimes involves more than simply removing the valve; it may require a full root replacement because the TAVR valve has healed through the wall of the root. These are complex, multicomponent operations.”
Advertisement
Paravalvular leak is more common with TAVR than with SAVR, but the incidence has decreased as TAVR device manufacturers have added valve skirts and enhanced valve dilation and as heart teams have improved their ability to choose the correct valve size. Another complication more common with TAVR versus SAVR is heart block that requires a new permanent pacemaker, Dr. Bakaeen points out. “This complication also has decreased over time thanks to better TAVR deployment that minimizes risk of injury to the heart’s conduction system,” he says.
As the incidence of TAVR valve deterioration has fallen, rates of endocarditis are rising. Cleveland Clinic is currently analyzing the incidence of endocarditis in TAVR versus SAVR, with results expected soon. “Looking at the raw data, there doesn’t appear to be a huge difference,” says Dr. Yun.
At Cleveland Clinic, patients being considered for TAVR see both a surgeon and an interventional cardiologist, who discuss the pros and cons of TAVR and SAVR before making a recommendation.
“Because of our experience with post-TAVR surgery, we understand that if we can provide a surgical solution to a patient’s problem at a younger age, we can focus on less-invasive options in older age,” Dr. Yun notes. “Of course, there are some cases where a younger patient is at high surgical risk and should be treated less invasively, but as a heart team we determine what’s best for an individual.”
The answer is not always clear, due to lack of long-term data for TAVR. “One issue we debate is what the expected durability of a TAVR valve will be in, for example, a 64-year-old,” Dr. Yun continues. “We expect the functional lifetime of a durable surgical aortic valve to be 12 to 15 years, on average, and the 10-year U.S. data for TAVR durability in low- and intermediate-risk patients will be very helpful when it becomes available.”
Advertisement
Since Cleveland Clinic surgeons are increasingly evaluating patients with previous TAVR for open-heart surgery, they plan to continue studying this population. “This clinical scenario is clearly part of the modern landscape,” says Dr. Yun. “These cases can be challenging, but at centers like ours, reasonable outcomes are feasible.”
“Due to the referral pattern at our institution, we likely see a skewed population,” Dr. Bakaeen adds. “Nevertheless, these data are a warning sign that TAVRs can fail early. We should be selective and think twice before performing TAVR in healthy, young patients. Our SAVR results have traditionally been exceptional, with zero mortality in the past 2 years, and they serve as a benchmark.”
Advertisement
Advertisement

Join us in New York City Dec. 5-6

Study examines data and clinical implications for performing Ross procedures in infancy versus later in life
Choice between smaller or larger prosthesis is a tradeoff between leak and pacemaker risks

4-D imaging informs complex aortic valve repair in adult and pediatric patients

BITA grafts themselves are rarely to blame, and outcomes can be good

TVT Registry analysis could expand indication to lower surgical risk levels

A scannable recap of our latest data in these clinical areas

Indication, timing and options for surgical intervention