Experience and strength in both SAVR and TAVR make for the best patient options and outcomes
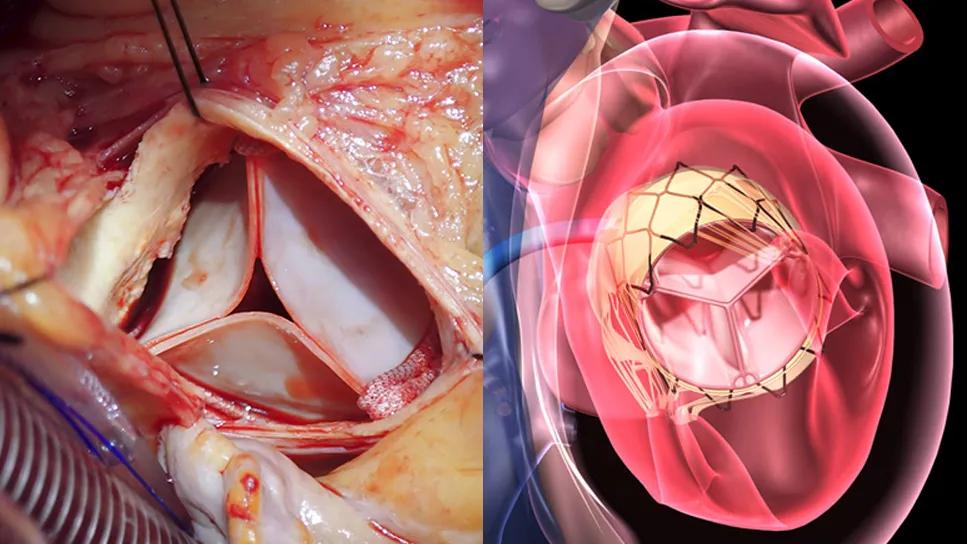
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9d8f394d-4e93-45d3-a716-99dc46f5117f/tavr-aortic-valve-combo)
side-by-side photo and illustration of bioprosthetic heart valves
For decades it has been recognized that higher volumes correlate with reduced operative mortality and complications in surgical aortic valve replacement (SAVR).1 This observation has been confirmed in more recent years, and a similar correlation has been seen with transcatheter aortic valve replacement (TAVR).2,3
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The general association between procedural volumes and positive outcomes is hardly new and is somewhat intuitive, yet the implications are not always fully appreciated.
For instance, the TVT Registry of the Society of Thoracic Surgeons (STS) and the American College of Cardiology shows that 100,501 commercial TAVR procedures were completed across 838 sites in the U.S. in 2023, for an average of 120 procedures annually per site. Since large centers perform many hundreds of TAVRs per year (Cleveland Clinic performs about 700), many sites are performing far less than 100 TAVRs per year to yield the overall average of 120. Some average little more than one per week, which can make it difficult for multiple operators to maintain optimal volumes and for the overall care team to develop expertise in the nuances of post-TAVR management.
The same phenomenon is also at play for isolated SAVR procedures, whose nationwide total of 18,792 in 2023 (according to the STS National Database) was far below the 100,000-plus TAVR procedures that year. This suggests an average of about 18 isolated SAVR procedures annually per STS cardiac surgery site in the U.S., with an even lower average count per individual cardiac surgeon.
In contrast, Cleveland Clinic performs among the highest annual volumes of SAVR and TAVR in the world, as reflected in Tables 1 and 2. Notably, even as isolated SAVR volumes have declined markedly nationwide in recent years with the growth of TAVR (down more than 37% from a peak of 30,171 in 2015, according to the STS National Database), Cleveland Clinic’s isolated SAVR volumes have increased in the past several years. As the tables reflect, these high SAVR and TAVR volumes have been associated with procedural mortality rates at least two to five times lower than expected rates or national benchmarks, along with TAVR complication rates similarly reduced from national benchmarks.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/820ffd2e-5610-4f0a-820c-a370debc2985/24-HVI-5368864-table1)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/308123c5-0b66-4647-b914-28a550372f22/24-HVI-5368864-table2)
Notably, because of the complexity of patients referred to Cleveland Clinic, the total number of aortic valve procedures is approximately 2,800 annually when one includes SAVR done in combination with coronary artery bypass, aortic surgery and double/triple-valve operations.
“Cleveland Clinic manages more patients with aortic stenosis than any other center,” says Samir Kapadia, MD, Chair of Cardiovascular Medicine. “This is despite not being located in one of the most densely populated parts of the country. Our long-standing reputation for leadership and excellent outcomes in aortic valve care consistently draws patients from all corners of the U.S. [as reflected in Figure 1] and all over the world.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/34bff2c6-7c63-4f6e-a8f6-4a6378af50e8/hvi-quality-service-map)
Figure 1. Each dot on the map depicts a patient who came to Cleveland Clinic for aortic valve care in 2022 or 2023, collectively representing a broad geographic draw.
Dr. Kapadia identifies three broad reasons why volume looms so large in the quality of aortic valve replacement (AVR) care.
“Experience matters not just for the technical skills of the surgeon or the proceduralist,” Dr. Kapadia says. “It has implications for how the whole care team manages the patient, such as when complications arise. It’s essential for optimal diagnosis of aortic stenosis and for determining the best timing of intervention. Our cardiologists have cared for so many patients with aortic stenosis that they have deep expertise in the use of multimodality imaging in this setting and how to factor other conditions, such as hypertrophic cardiomyopathy or cardiac amyloidosis, into treatment strategies.”
Experience is particularly important for patients who have other cardiac conditions in addition to aortic stenosis. “Many of our patients requiring AVR have coronary disease, mitral valve disease and other heart conditions that need to be addressed at the same time,” says cardiothoracic surgeon Lars Svensson, MD, PhD, Chief of Cleveland Clinic’s Heart, Vascular and Thoracic Institute. “For instance, we perform nearly 200 combined SAVR and CABG operations each year, not to mention multivalve operations and SAVR combined with aortic surgery. These patients particularly benefit when they are managed by teams who perform these complex procedures often.”
Advertisement
Dr. Svensson notes that failure to address concomitant heart conditions at the time of AVR is increasingly a problem with the recent growth of TAVR. “In addition to cases of failed TAVR, we see growing numbers of patients who come to us fairly soon after having TAVR elsewhere,” he says, “because they have progression of other heart disease that was present at the time of their TAVR, such as coronary disease or other valve disease.”
High-volume heart valve programs are also best equipped to offer patients the most appropriate option for management of their particular case of aortic stenosis and any related conditions. “High-volume programs tend to have the most valve types available for both SAVR and TAVR and the most experience in using all of them,” Dr. Kapadia says. “This allows us to precisely match valves to patients’ anatomic needs. A high-volume program like ours is also able to offer true lifetime management of aortic valve disease, including options such as the Ross and Ozaki procedures, homografts, aortic valve repair and reimplantation, aortic root replacement and annular enlargement, valve-in-valve procedures, TAVR valve explantation, the BASILICA procedure and more.”
Centers that have disproportionate experience with either TAVR or SAVR can tend to steer patients to the option they are most experienced and comfortable with rather than what is best for the patient’s individual situation. “When a program has deep experience with both procedures, this is not a concern,” Dr. Kapadia notes.
Advertisement
In fact, an analysis of a large Medicare database from a few years ago found that hospitals’ total SAVR volumes were correlated with TAVR outcomes, with higher 30-day and one-year TAVR mortality seen at low-volume SAVR hospitals.4
“Just as having an experienced TAVR program improves SAVR outcomes by treating the highest surgical risk patients, the converse is also true that better SAVR makes for better TAVR,” Dr. Svensson wrote in an editorial he co-authored to accompany the study.5 “The two procedures are inextricably intertwined as part of a comprehensive disease management program for the management of aortic stenosis.”
1. Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128-1137.
2. He J, Zhang Z, Wang H, et al. The relation between volume and outcome of transcatheter and surgical aortic valve replacement: a systematic review and meta-analysis. Cardiovasc Ther. 2020;2020:2601340.
3. Vemulapalli S, Carroll JD, Mack MJ, et al. Procedural volume and outcomes for transcatheter aortic-valve replacement. N Engl J Med. 2019;380:2541-2550.
4. Hirji SA, McCarthy E, Kim D, et al. Relationship between hospital surgical aortic valve replacement volume and transcatheter aortic valve replacement outcomes. JACC Cardiovasc Interv. 2020;13(3):335-343.
5. Mack MJ, Svensson L. Why does more SAVR make better TAVR? JACC Cardiovasc Interv. 2020;13(3):344-345.
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Experience-based takes on valve-sparing root replacement from two expert surgeons
30-year study of Cleveland Clinic experience shows clear improvement from year 2000 onward
Surgeons credit good outcomes to experience with complex cases and team approach
For many patients, repair is feasible, durable and preferred over replacement
In experienced hands, up to 95% of patients can be free of reoperation at 15 years
Ideal protocols feature frequent monitoring, high-quality imaging and a team approach
20 years of Cleveland Clinic experience in ~500 patients with proximal aortic aneurysm or dilation