Older Psoriasis Patients May Experience Quicker Transition

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/defef6b2-06c0-4c81-9077-48fb74b934e8/Hand-Wrist-Elbow-Pain-1354565598-770x533-1_jpg)
Psoriatic arthritis
By M. Elaine Husni, MD, MPH, and Shashank Cheemalavagu, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Psoriatic arthritis (PsA) is a condition that affects up to 30% of individuals with psoriasis (PsO). Typically, PsA emerges seven to 10 years after the onset of PsO. However, the timing of transition can vary significantly, leading to delays in diagnosis and high rates of undiagnosed PsA. In this study, we aim to identify clinical and demographic factors associated with the time it takes for PsO to transition to PsA.
In our longitudinal psoriatic disease cohort, we identified individuals with both PsO and PsA diagnoses. We measured the duration between the dates of PsO and PsA diagnosis, treating it as a continuous outcome variable using multivariable linear regression analysis. Our list of candidate predictors included: sex, age at PsO diagnosis, family history of PsO, BMI, treatment, cardiovascular disease, hypertension, diabetes, dyslipidemia, nail involvement, Dermatology Life Quality Index (DLQI), elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), alcohol use and smoking habits.
We also created a subgroup model utilizing individual data with body surface area (BSA) data, and narrowing down the predictors to age at PsO diagnosis, smoking habits, elevated ESR/CRP, BMI, and family history of PsO. Model results were presented using coefficient estimates and respective 95% confidence intervals. Variables were also ranked based on their relative contribution to the models, as assessed by Akaike Information Criterion (AIC). All tests were two-sided, assuming an alpha level of 0.05.
Advertisement
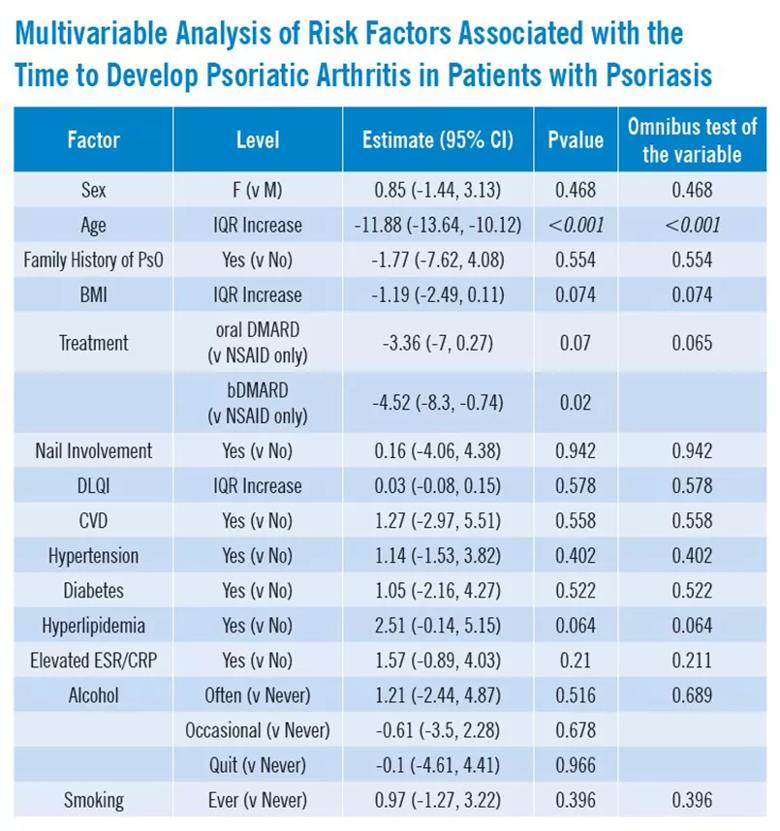
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9187c7d3-661d-4e9a-8c95-90ad6f1eddd0/23-RHE-4333863-CQD-inset1_jpg)
Our analysis included a cohort of 384 patients with a median age at PsO diagnosis of 30.4 years, and 52.2% of patients were female. Importantly, we found that age at diagnosis of PsO is significantly linked to the time it takes for PsO to progress to PsA. For example, when patients reach an age of around 42 (Q3), they experience, on average, approximately 12 fewer years between their PsO to PsA diagnoses compared to patients diagnosed at 18.9 years (Q1), even after controlling for relevant variables in the model (-11.88 (-13.64, -10.12); p < 0.001).
Furthermore, our findings regarding use of biologic disease-modifying anti-rheumatic drugs (bDMARDs) revealed that these individuals tend to experience a shorter time frame, averaging 4.5 fewer years between PsO to PsA compared to patients on NSAIDs only, after controlling for other variables in the model (-4.52 (-8.3, -0.74), p = 0.02).
Although the use of bDMARDs demonstrates a trend toward shorter transition period (4.5 years) compared to non-bDMARDs, the overall effect of treatment was not statistically significant. Similarly, patients with BSA of 5% (Q3) have on average 1.1 more years from PsO to PsA than patients with BSA of 0.5% (Q1) after controlling for other variables in the model (1.11 (-0.44, 2.65), p = 0.16), although the overall effect of BSA is not statistically significant.
The analysis revealed that the most influential factor in the model, as indicated by the AIC, was the age at which PsO was diagnosed. An AIC score exceeding or equal to 2 suggests a statistically enhanced model, thus emphasizing the value of incorporating age as a variable in the model.
Advertisement
Our study offers compelling evidence that the age at which psoriasis first appears serves as an important predictor for the transition from psoriasis to psoriatic arthritis. Older individuals diagnosed with PsO tend to progress to PsA more rapidly. The time difference is not only statistically significant but also carries crucial clinical implications. Compared to their younger patient cohort (diagnosed at 18.9 years, Q1), older patients (diagnosed at 42.6 years, Q3) develop PsA an average of 12 years sooner.
Advertisement
Advertisement
Unraveling the TNFA receptor 2/dendritic cell axis
Nasal bridge inflammation, ear swelling and neck stiffness narrow the differential diagnosis
Genetic testing at Cleveland Clinic provided patient with an updated diagnosis
From dryness to diagnosis
Multiple comorbidities are associated with pediatric psoriasis
Untreated seropositive erosive RA led to peripheral ulcerative keratitis
New clinic meets Hispanic patients where they are
Treatment strategies require understanding of pathomechanisms