Advanced transcatheter options have expanded patient candidacy
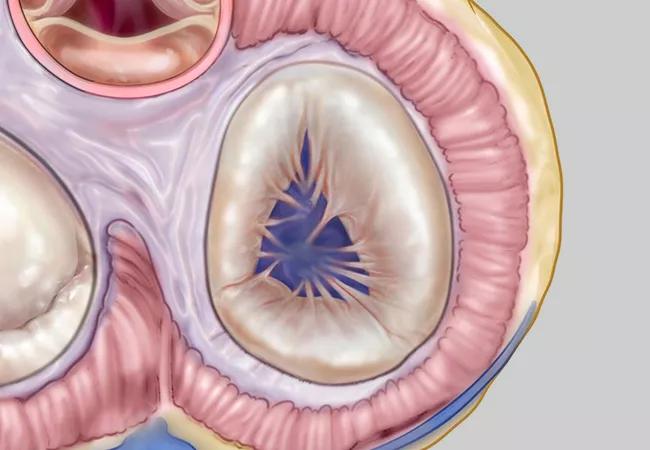
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/06606651-4ee7-42f9-8e5f-518030fe6e47/22-HVI-3413075_illustration-of-pulmonary-valve_650x450_jpg)
22-HVI-3413075_illustration-of-pulmonary-valve_650x450
Four transcatheter systems are now available for pulmonary valve replacement (PVR), accommodating right ventricular outflow tract (RVOT) abnormalities up to a diameter of 38 mm. This minimally invasive approach to PVR is a safe and effective alternative to open surgery, but until recently, the endovascular option was limited to patients with an RVOT diameter up to 22 mm.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“When we see adults with pulmonary valve (PV) dysfunction who need an intervention, we always try to determine if they are a candidate for a transcatheter approach,” says cardiologist Joanna Ghobrial, MD, MS, Medical and Interventional Director of the Adult Congenital Heart Disease Center at Cleveland Clinic. “Often these patients — especially those with congenital disease — have had multiple prior open-heart surgeries, so we try to limit additional risk. The overall goal is to minimize how many open-heart surgeries a patient undergoes in a lifetime, and transcatheter PVR is the way to do this. Furthermore, transcatheter PVR is the best option in patients deemed too high-risk for surgery due to other comorbidities.”
In most cases, PV disease results from a congenital heart defect. PV stenosis or regurgitation associated with tetralogy of Fallot is the most common cause, followed by isolated congenital PV stenosis. Other conditions include pulmonary atresia, truncus arteriosus and transposition of the great arteries.
PV dysfunction can also be acquired. Patients with congenital aortic stenosis who have undergone a Ross procedure in the past (i.e., replacement of the PV in the aortic position, then homograft placement in the pulmonary position) tend to develop prosthetic PV dysfunction years later. Other examples of acquired PV disease include postinfectious or inflammatory disease.
Many adults with congenital heart defects may have typical symptoms of cardiac insufficiency. However, some are asymptomatic or may not know that they are limited, especially if they have been adjusting to it all their life, Dr. Ghobrial explains. This makes subjective history unreliable, and regular metabolic stress testing is indicated in all adults with a history of congenital heart disease or who have had a previous valve operation. For either a regurgitant or a stenotic PV, an ECG and echocardiogram are essential for evaluation, followed by an MRI or CT, especially if echo windows are inadequate. MRI is excellent at assessing right heart size and function, and CT is key in assessing candidacy for transcatheter PVR. Cardiac catheterization may be indicated for more thorough assessment.
Advertisement
“It’s critical that patients in need of an intervention be referred to a center with Adult Congenital Heart Association (ACHA) accreditation,” Dr. Ghobrial urges. “Advanced transcatheter options now can cover a broad array of anatomies, and if surgery is needed instead, a high-volume center can offer this strategy with very low risk.”
For patients with congenital PV stenosis, balloon valvuloplasty may offer adequate relief without PV replacement for some time.
Valve replacement should be considered for PV regurgitation with marked right ventricular dilation or dysfunction, left ventricular dysfunction, or an arrhythmia such as nonsustained ventricular tachycardia.
The Melody and Sapien valves are well-established balloon-expandable systems that can safely be used in RVOTs up to 29 mm in diameter.
In the past two years, two advanced devices have expanded options for patients with severe PV regurgitation:
“When surgery is indicated instead of an endovascular strategy, we can assure patients that PVR is usually a straightforward operation,” says Cleveland Clinic pediatric and congenital heart surgeon Tara Karamlou, MD, MSc, Surgical Director of the Adult Congenital Heart Disease Center. “For most patients who have had a previous valve operation, we can enter through their prior incision, and patients can expect a three- to five-day hospital stay and short convalescence.”
Advertisement
She adds that Cleveland Clinic surgeons prefer using a bioprosthetic porcine valve with a large diameter (25 or 27 mm). These valves have proved to be the most durable and set the stage for a valve-in-valve transcatheter option down the road if further intervention is needed. Reoperation for future PV problems is rare. No long-term anticoagulation therapy is required, although aspirin is recommended for six months after the operation.
Dr. Karamlou notes several situations in which surgery is preferred over a transcatheter approach:
Regardless of PVR approach, patients require lifelong annual monitoring afterward. Periodic echocardiography is usually adequate, but cardiac MRI may also be needed. Patients will also need infective endocarditis prophylaxis, including antibiotics for dental visits.
Patients receiving a transcatheter valve often have aspirin with or without clopidogrel prescribed for a short time after the procedure; lifelong aspirin therapy is generally indicated.
Both Drs. Ghobrial and Karamlou emphasize the value of the team approach used at Cleveland Clinic, which ensures that surgeons and interventionalists together evaluate the best treatment strategy for each patient.
Advertisement
“We have learned important lessons about how to successfully handle complex patients from our multidisciplinary experience,” says Dr. Ghobrial. “Because our different specialties routinely collaborate, patients can count on an unbiased strategy that is in their best interest.”
Dr. Karamlou, who performs surgeries on patients of all ages, adds that Cleveland Clinic is one of few integrated centers that specialize in congenital heart disease in both pediatric and adult populations. “Having this wide spectrum of expertise gives us a good understanding of the consequences of cardiovascular defects over the lifespan,” she says. “This is a real advantage in caring for these complex patients.”
Advertisement
Advertisement
HALT has unique clinical implications for adults with congenital heart disease
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon
How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR