Targeted IL-1 blockers and CMR techniques allow more-tailored treatment strategies
The diagnosis and management of recurrent pericarditis have advanced dramatically since European guidelines were last published more than seven years ago. Important new evidence has emerged supporting earlier treatment with interleukin-1 (IL-1) blockers and the use of cardiac magnetic resonance imaging (CMR) for diagnosis, risk stratification and treatment decisions. These developments have produced a paradigm shift in management of recurrent pericarditis while also opening exciting new avenues of research. So concludes a team of Cleveland Clinic clinician researchers in a newly published narrative review of the condition in JAMA Cardiology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The emergence of advanced imaging — including echo as well as CMR — as a comprehensive diagnostic and monitoring tool and the addition of IL-1 blockers to the treatment armamentarium have significantly changed our ability to manage this very difficult condition,” says the review’s corresponding author, Allan Klein, MD, Director of the Center for the Diagnosis and Treatment of Pericardial Diseases at Cleveland Clinic and Past President of the American Society of Echocardiography. “Our review provides a state-of-the-art algorithm for pericarditis management and urges professional societies to upgrade their guidelines on diagnosis and treatment.”
While echocardiography is recommended as the first imaging test for evaluating pericardial disease, guidelines typically reserve more-advanced imaging methods, such as CMR and CT, for cases in which the diagnosis is unclear. But CMR has evolved in recent years, with potential benefits for using it much earlier in the process for patients with complicated pericarditis.
Similarly, traditional treatment of recurrent pericarditis — a combination of anti-inflammatory drugs including NSAIDs, colchicine and prednisone — often leads to steroid dependence, with many patients needing years of therapy, and accompanying side effects. The advent of new effective and targeted therapies, such as IL-1 blockers, is changing best treatment strategies.
To update physicians on current diagnostic and therapeutic approaches to recurrent pericarditis, the review’s authors emphasized developments since publication of the 2015 European Society of Cardiology (ESC) guidelines on pericardial disease. They searched PubMed and Cochrane databases for relevant publications up to April 2022. Major highlights of the review are briefly summarized below.
Advertisement
Information gleaned from CMR can help with diagnosis, monitoring and management of pericardial disease. CMR allows for assessment of pericardial anatomy and cardiac hemodynamics, characterization and quantification of pericardial effusion, and disease staging.
Pericardial tissue characterization — i.e., detailing anatomy and histopathology to identify the presence and stage of pericardial inflammation — forms the basis for personalized therapy. It is assessed mainly using late gadolinium enhancement (LGE) and edema-weighted T2 STIR sequences (Figure)
The presence of both LGE and pericardial edema on T2 STIR imaging has a sensitivity of 73% and a specificity of 99% for recurrent pericarditis, which is superior to the diagnostic yield of clinical criteria alone. “These CMR features can better establish the diagnosis of recurrence compared with conventional clinical criteria, suggesting that they should be added to diagnostic scores,” Dr. Klein urges.
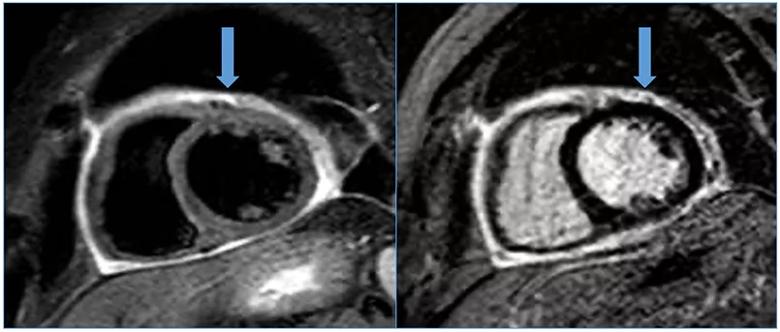
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5fab05a9-d2fa-409c-97f8-8517298c1271/22-HVI-3073724-CQD-INSET_jpg)
Figure. CMR images providing tissue characterization of a patient with active recurrent pericarditis. On the left is a T2W STIR image; on the right is an LGE image.
Moreover, CMR can also help determine prognosis and steer therapy. Decisions for starting, escalating, tapering and stopping anti-inflammatory treatment depend on the extent of inflammation. “The magnitude of pericardial delayed hyperenhancement informs the expected clinical course and provides insights into the appropriate duration of treatment,” notes review co-author Paul Cremer, MD, staff cardiologist in the Section of Cardiovascular Imaging.
Advertisement
Anti-inflammatory medications currently form the backbone of recurrent pericarditis treatment. “We see patients who receive these medications for 3 to 4 years, eventually becoming dependent on corticosteroids and colchicine for relief of their chest pain,” says review co-author Sachin Kumar, MD, senior resident at Cleveland Clinic.
The most recent options — IL-1 blockers — have demonstrated marked efficacy and are currently recommended for infection-negative, corticosteroid-dependent disease that is not responsive to colchicine. The first IL-1 blocker to gain FDA approval for recurrent pericarditis was rilonacept in 2021, following the pivotal RHAPSODY trial (N Engl J Med. 2021;384:31-41) led by Dr. Klein.
Anakinra has since become an additional option, although its use for recurrent pericarditis is off-label. Use of anakinra in this setting has been supported by the AIRTRIP randomized trial in Europe.
Although all the IL-1 blockers are costly, the review authors identify a clear role for these agents in the management of patients with multiple recurrences. In a treatment algorithm provided in the review, they recommend IL-1 inhibitor therapy instead of corticosteroids in patients with recurrent pericarditis who have a high C-reactive protein level and are positive for LGE despite NSAIDs and colchicine treatment.
They also urge further research to better define the use of IL-1 blocker therapy.
Complete radical pericardiectomy is reserved for patients with recurrent pericarditis with debilitating symptoms despite medical therapy. For patients with constrictive disease without signs of inflammation on CMR or who have pericardial calcification on cardiac CT, the condition is likely irreversible, indicating the need for radical pericardiectomy. In the past, pericardiectomy was thought to have a high operative risk of 6% to 18%, but recent reports from specialized centers suggest the risk is dependent on the causes and comorbidities, with operative mortality less than 1.5%.
Advertisement
“We have found that the timing of surgery, preferably when the inflammatory markers are normal, makes the operative approach somewhat technically easier, while the etiology of pericarditis is one of the most important factors influencing outcomes,” observes Cleveland Clinic cardiothoracic surgeon Marijan Koprivanac, MD. “As diagnostic tools and medical management have evolved, so has the surgical approach. Historically, we believed that partial pericardiectomy (“phrenic to phrenic”) was sufficient to relieve constriction and patients’ symptoms, but over time we learned that many patients returned for re-excision of remaining pericardium. Consequently, complete radical pericardiectomy has become the treatment of choice for patients with pericarditis refractory to medical management.”
In addition to proposing a new integrated approach to pericarditis using advanced cardiac imaging and IL-1 inhibitors, the review provides extensive tables comparing various imaging methods for use in pericarditis, describing the spectrum of pericarditis with regard to imaging features and treatment practices, and summarizing key clinical trials of therapies.
“Recent advances have real-world clinical implications and should now be incorporated into practice guidelines,” concludes Dr. Klein. “Better standards are critical to providing accurate diagnosis of patients with recurrent pericarditis and helping them avoid long-term complications of steroids with the new targeted therapies.”
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon
How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR
Optimal management requires an experienced center