Complex procedure highlights the power of coordinated care across spinal, thoracic and vascular surgery

A 33-year-old patient has made a full recovery following the removal of a large nerve tumour from a complex area at the intersection of his spine, lung and major arteries.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
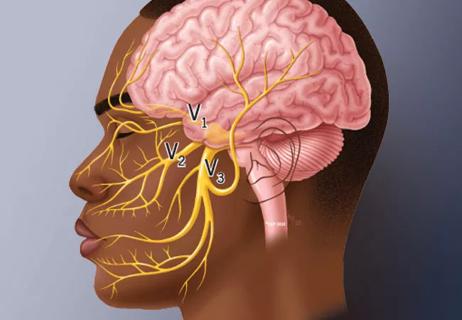
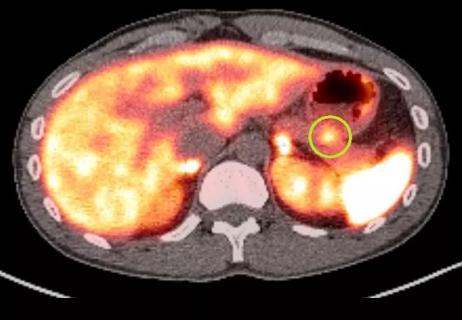
The tumour was reported as an incidental finding on a chest X-ray for a suspected broken rib. Diagnosed as a grade 1 schwannoma arising from the spine, the noncancerous tumour was notable for its size (7 cm) but more importantly for its rare location (extending to the superior mediastinum at the apex of the lung and adjacent to the carotid, subclavian and vertebral arteries).
Because of the tumour’s high-risk location, an outside hospital advised surveillance since the patient was asymptomatic. One year later, however, the tumour had grown and was at risk of compressing the spinal cord, lung and major arteries, making the surgery even riskier.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e6b7739e-9a6b-4080-a7cd-db92f47e0f84/25-REG-6761958-2-Schwannoma)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/af29ccae-35bb-46be-8e73-409873d59e80/25-REG-6761958-4-Schwannoma)
Imaging depicting the 7 cm schwannoma in the superior mediastinum
After consultations at multiple hospitals, the patient chose treatment at Cleveland Clinic London.
“Some hospitals turned him away because of the difficulty and rarity of the surgery,” says George Prezerakos, MD, PhD, a consultant spinal neurosurgeon at Cleveland Clinic London. “The tumour was in a dense anatomical area, with important nerves and large blood vessels confined in a tight, difficult-to-access bone space. Plus, it was in a no-man’s-land bordering the domains of thoracic, vascular, spinal, and head and neck surgeons.”
Ultimately, it was Cleveland Clinic London’s unified team of specialty surgeons that attracted the patient.
“We also understood how important the surgery would be to him as a professional guitarist who needed to maintain function of his left arm,” Mr Prezerakos says. “We discussed options, including removing the tumour from the back, which would be difficult visually and disrupt muscles and bones, or from the front, which would require a sternotomy.”
Advertisement
Mr Prezerakos opted to proceed with a posterior, parascapular surgical approach (between the spine and shoulder blade), reserving the anterior approach as a secondary option.
“One of our main goals was to prevent any neurological deficit, knowing that even a bit of numbness could ruin this patient’s career,” Mr Prezerakos says. “Even accessing the area, detaching the muscles and resecting a small part of the bones and ribs, could cause shoulder deformity, dysfunction and chronic pain that could alter his life.”
In addition to Mr Prezerakos, the surgical team included consultant thoracic surgeon Nikolaos Panagiotopoulos, MD, PhD, and consultant vascular surgeon Richard Gibbs, MB ChB, MD. In addition, specialists from University College London created 3D anatomical models to help the surgeons plan the procedure with precise mapping of critical anatomy.
“The 3D models added significant value by helping us visualise the anatomy, including the bones’ and large vessels’ relationships to the tumour, rather than going by a mental picture or textbook image,” Mr Prezerakos says.
One model was an almost life-size representation of the patient’s bony anatomy. A second, smaller model added representation of the patient’s blood vessels.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/828db347-4e25-416b-ad57-fbb31d5ee004/25-REG-6761958-3-models)
Life-size 3D model of the patient’s bony anatomy (left) and smaller 3D model including representation of the patient's blood vessels (right)
“Working with these models helped us plan various aspects of the procedure, such as how much muscle to detach in the back so we could remove a portion of the ribs, deflate the lung and access the back of the tumour,” Mr Prezerakos explains. “We wanted to minimise disruption of the shoulder blade since it is the attachment for many muscles and is integral to the movement of the shoulder and arm. So, the models helped us navigate well in the cavity, where few surgeons have encountered a tumour of this magnitude and complexity.”
Advertisement
For a surgical procedure in this specific anatomic location, spinal robotic navigation would be of little use because of the depth and confined space, he adds.
During the six-hour operation, Mr Prezerakos accessed the spine and spinal cord, placed metalwork to strengthen it, separated the tumour from the nerves, and created the surgical corridor through the back muscles and ribs to the roof of the chest cavity. Mr Panagiotopoulos entered with a thoracoscopic camera, which improved visual access. Together the surgeons removed the tumour from the lung and vessels.
Prof Gibbs was present from the beginning in case of injury to a major artery or in case a secondary anterior approach became necessary, which would have required maneuvering around major arteries. He stepped in when the tumour was dissected from the anterior, deep attachments to the great vessels.
“The final part of the operation was particularly demanding,” Mr Prezerakos says. “The tumour was approached from the back, and its proximity to major blood vessels at the front could not be directly seen. Despite this, the tumour was removed completely, in one piece, while preserving the surrounding muscles and the key nerves and blood vessels of the shoulder and neck.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fe251a93-9f91-45ca-a167-0f352b18c5ed/25-REG-6761958-4-excised-tumour)
Excised tumour, the size of a peach
The complete excision left the patient with no functional or neurological deficits.
“The first thing the patient did when he opened his eyes after surgery was to lift his left hand and wiggle his fingers,” Mr Prezerakos says. “His function was completely intact with no tingling or numbness.”
Advertisement
Despite early postoperative pain, the patient recovered quickly with help from shoulder physiotherapy. Eight weeks later, he returned to playing guitar and touring with his band.
This case exhibits the power of multidisciplinary coordination and the value of 3D modelling when addressing conditions that require innovative planning and precision.
“Few specialist centres could have handled this case individually,” Mr Prezerakos says. “It was an extensive tumour in a unique area. The patient sought care from many leading institutions but ultimately chose Cleveland Clinic London, a testament to our clinical expertise, team-based approach and patient-centred care.”
Advertisement
Advertisement

Patient with cerebral palsy undergoes life-saving tumor resection

UK experts compare and contrast the latest recommendations

Advances in imaging technology could offer new insights for combatting age-related muscle loss

Case report of a young man with severe traumatic brain injury and cognitive deficits

Special glasses allowed surgeon to see 3D models and anatomic data superimposed on surgical field

First private hospital in the U.K. to receive HIMSS EMRAM Stage 6 accreditation
A review of takeaways from the recent U.K. national guidelines
Patient’s unexplained low blood glucose levels in the absence of diabetes spark quest for answers