Catheterization increases risk, but no significant difference between methods
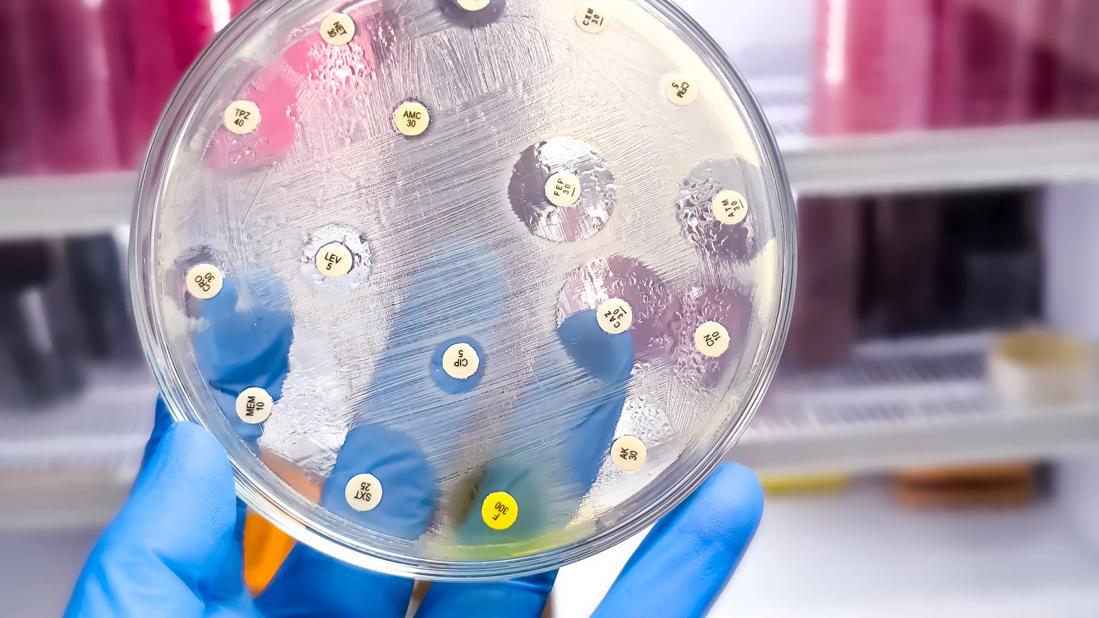
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/34135a98-d532-4549-9609-6f89316db4ff/antibiotic-susceptibility-test-2157592829)
Antibiotic test
Method of catheterization, whether indwelling or intermittent, does not appear to impact a woman’s risk of developing a urinary tract infection (UTI) following labor, according to a recent study.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Few studies have attempted to determine which method of catheterization is associated with increased risk of UTI. Those that have were either not powered to reveal a difference in the rate of infection, or assessed rates of bacteriuria and not UTI, according to Oluwatosin Goje, MD, an Ob/Gyn and fellowship-trained reproductive infectious diseases specialist with Cleveland Clinic.
“The existing literature did not directly address which method of catheterization is associated with less risk, so we conducted this study to determine the risk of UTI in laboring patients that were exposed to intermittent catheterization compared with the routine indwelling catheter,” says Dr. Goje, a co-author on the paper that was published in The Journal of Maternal-Fetal & Neonatal Medicine.
“There are generally two viewpoints when it comes to selecting a catheterization method for laboring women,” Dr. Goje explains. “There are those who use a Foley catheter after an epidural is placed and leave it in place for the remainder of the labor and delivery; and there are those who prefer intermittent catheterization. There are infection risks with both methods. With the Foley, leaving a foreign body in for potentially long periods of time can be viewed as a nidus for infection. The risk with intermittent catheterization is that each catheter insertion creates an avenue to introduce bacteria from a laboring bed that maybe unsanitary.”
For the study, investigators searched a large obstetric database of patients who delivered vaginally at full-term (≥ 37 weeks 0 days gestational age) between January 2013 and December 2016 at Cleveland Clinic birthing hospitals, and then used diagnosis codes from the ICD-9 and ICD-10 to identify patients who were diagnosed with UTI within the first 30 days following delivery.
Advertisement
Patients (N = 166) who were diagnosed with UTI based on symptoms and a positive urine culture or abnormal urinalysis (if available) were compared with controls who were not diagnosed with or treated for a UTI within the first 30 days postpartum (N = 695). Of the entire sample, 67.0% underwent catheterization either intra- or post-partum, and 25.7% underwent catheterization at both points. Among intra-partum catheterizations, 31.9% were indwelling; 5.0% of postpartum catheterizations were indwelling.
“Although patients who had any type of catheterization were 2.61 times more likely to develop a UTI compared with those without catheter use, there were no significant difference in UTI rates based on catheterization method,” says Dr. Goje.
“Our analysis did identify two predictors of UTI. Women who had at least one UTI in pregnancy were 2.57 times more likely to develop a UTI. Duration of labor also approached significance as a predictor of UTI risk: longer labors increased odds of UTI by 3% per hour among patients who received catheters,” Dr. Goje explains.
These results highlight the importance of treating patients for UTIs developed during pregnancy. According to Dr. Goje, physicians should have a low threshold for treating patients whose baseline urine cultures reveal asymptomatic bacteriuria (ASB) in pregnancy.
“Depending on the patient’s immune system, an untreated UTI in a pregnant woman can lead to ascending infection — pyelonephritis and its sequelae of preterm contractions, premature labor and preterm delivery, and there is risk for developing acute respiratory distress syndrome,” in severe cases says Dr. Goje. “Unrecognized or untreated UTI in postpartum women can lead to ascending infection of the urinary tract and possible urosepsis, which if left untreated can lead to septiciemia. For these reasons, obstetricians/midwives should follow the guidelines of screening for ASB in pregnancy. I recommend treating ASB in pregnancy, along with careful attention to hygiene protocols and follow-up following intra- or post-partum catheterization.”
Advertisement
Advertisement
A Q&A with Cleveland Clinic’s board-certified pediatric and adolescent gynecologist
Increasing uptake remains a challenge
Multidisciplinary teams work together in in-situ scenarios
Uterine transposition cleared the field for radiation therapy
ACOG-informed guidance considers mothers and babies
Prolapse surgery need not automatically mean hysterectomy
Artesunate ointment shows promise as a non-surgical alternative
New guidelines update recommendations