Proper diagnosis and treatment require a careful mix of patient and clinical considerations
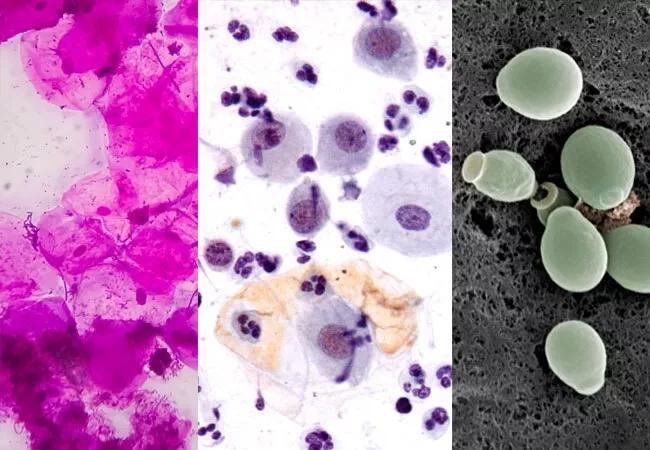
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a17aabdb-92bb-4605-a2b7-2bd8d23b8b9a/21-WHI-2515076_CQD_650x450_combination_jpg)
Vaginitis diagnosis
Vaginitis affects millions of women and accounts for more than 10 million office visits to physicians annually. Yet it is frequently misdiagnosed, and opinions vary on the most appropriate diagnostic pathway.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Vaginitis is a broad term used to describe any disorder of the vagina that causes irritation and inflammation,” says Oluwatosin Goje, MD, MSCR, FACOG, a specialist in reproductive infectious diseases and vulvar and vaginal disorders in the Ob/Gyn & Women’s Health Institute at Cleveland Clinic. “But when we talk about infectious vaginitis, there are three main types – bacterial vaginosis, candidiasis and trichomoniasis.”
Proper assessment and diagnosis of vaginal infections are critical to reducing the potential for recurrent and persistent infections.
“Misdiagnosis and self-treatment are more expensive for patients and for the health system than diagnosing and treating infectious vaginitis from the get-go,” says Dr. Goje. “It’s also the reason the feminine aisles in stores are crowded with products to balance the vaginal milieu. Patients keep looking for some relief, and marketers prey on them.”
While vaginal infections can produce an array of similar symptoms, such as increased discharge and itchiness, each of the three main causes have distinct traits, effects and treatments.
Advertisement
Mixed infections and co-infections add to the challenge of accurately diagnosing vaginitis. With mixed infections, two types of vaginitis contribute to the symptomology and cause the same infection. For example, a patient may have BV and CV. If a physician only tests and treats for BV because of a malodorous smell and vaginal discharge, the infection will remain.
A co-infection is a simultaneous infection caused by multiple pathogen species, with one playing a larger role and causing the clinical symptoms. For instance, a patient may have BV and chlamydia, which is generally asymptomatic.
Accurately diagnosing vaginitis requires testing to determine the etiology of vaginal symptoms. While private companies offer super tests that use one swab to ascertain the cause of vaginitis, these tests are expensive and often not covered by insurance.
“We prefer to use tests that do separate things,” says Dr. Goje. “At Cleveland Clinic, we have a swab for gonorrhea and chlamydia, and we have a swab for trichomoniasis, BV and Candida because many times those three cause a mixed infection.”
Physicians need to listen closely to patients and use their critical-thinking skills to decide on the appropriate diagnostic pathway.
“Break down the testing if you think the symptoms and clinical features point toward a certain thing,” says Dr. Goje. She offers the following advice:
Advertisement
Challenges to properly diagnosing and treating vaginitis are compounded by societal attitudes. “Because vaginitis is a hush-hush topic, we have not had rapid advancements in the field compared to cancer, diabetes or hypertension,” says Dr. Goje.
She convened an expert panel of physicians to examine current issues and diagnostic challenges related to vaginitis in the Oct. 18, 2021, issue of Population Health Management. The article includes an algorithm to help clinicians in the decision-making process.
Dr. Goje stresses that patient education is equally important.
“Educating women empowers them to understand what is going on with their bodies. It validates them and reinforces that they don’t have to be secretive or ashamed,” she says. “Patient education is the best preventive mechanism.”
Dr. Goje offers a final piece of advice to physicians: “If you have tested a patient for everything and there is no infection but the patient is still symptomatic, don’t dismiss them,” she says. “Refer them to a vaginitis specialist.”
Advertisement
Advertisement
Multidisciplinary teams work together in in-situ scenarios
Uterine transposition cleared the field for radiation therapy
ACOG-informed guidance considers mothers and babies
Prolapse surgery need not automatically mean hysterectomy
Artesunate ointment shows promise as a non-surgical alternative
New guidelines update recommendations
Two blood tests improve risk in assessment after ovarian ultrasound
Recent research underscores association between BV and sexual activity