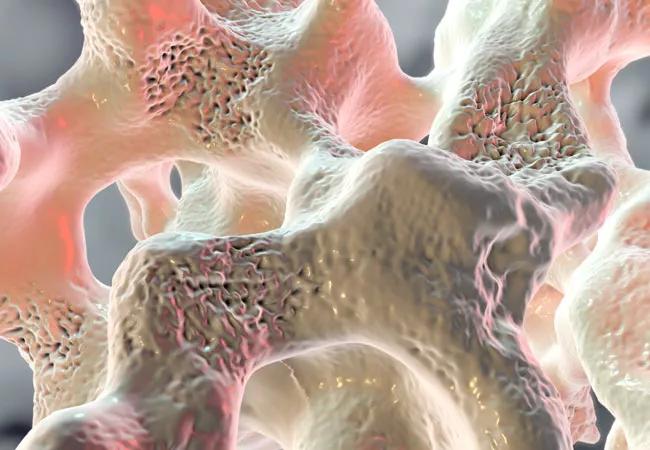
Dual-acting drug increases bone formation while decreasing resorption
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A new anabolic agent for the treatment of postmenopausal women at high risk for fracture was approved by the FDA in April 2019.
Romosozumab is a monoclonal antibody against sclerostin, a cytokine produced mostly by osteocytes that regulates bone formation. The Wnt signaling pathway controls osteoblast formation and activity; sclerostin is an inhibitor in the pathway. Sclerosteosis is a rare disease caused by a genetic defect in the gene that codes for sclerostin. Patients with sclerosteosis have very high bone mass and are fracture resistant since osteoblast activity is upregulated in the absence of sclerostin. Romosozumab has the effect of removing sclerostin and upregulates bone formation.
Unlike the parathyroid hormone (PTH) analogs (teriparatide and abaloparatide), which increase both formation and resorption, romosozumab increases formation and decreases resorption; hence, the “dual effect” noted in the label. In clinical trials, this resulted in a large bone build. The drug is given once per month as two subcutaneous injections for 12 months, and is paid under Medicare B plans.
Romosozumab was approved following three clinical trials: the FRActure study in postmenopausal woMen with ostEoporosis (FRAME), the Active-contRolled FraCture study in postmenopausual women with osteoporosis at High risk of fracture (ARCH) and the STudy evaluating effect of RomosozUmab compared with teriparatite in postmenopaUsal women with osteoporosis at high risk for fracture pReviously treated with bisphosphonatE therapy (STRUCTURE). FRAME compared romosozumab to placebo for 12 months, followed by an additional 12 months of denosumab in all patients.1 Vertebral fractures were reduced by 73% at 12 months and 75% at 24 months in the romosozumab/denosumab arm. However, there was not a significant nonvertebral fracture reduction, which was felt to be a result of the low baseline fracture risk in the trial (most patients had FRAX 10-year risk that was less than the NOF treatment thresholds). This may be in part due to the geographic distribution of the patients, as 39% were Latin American where fracture risk is much lower than in Caucasian groups. A post-hoc analysis excluding Latin American patients shows a significant non-vertebral fracture reduction.
Advertisement
ARCH was an active comparator trial: 12 months of romosozumab vs 12 months of alendronate, followed by 12 months of alendronate in all patients.2 Patients in this trial had a much higher risk for fracture than those in the FRAME trial. The risk reduction for patient on romosozumab was 0.5 (50%) for vertebral fracture, and 0.62 (38%) for hip fracture. Remember that alendronate reduced vertebral and hip fracture in its registration trial by 50%. An unexpected cardiovascular signal occurred in ARCH — an increase in major adverse cardiovascular events (MACE – MI, stroke and cardiovascular death; relative risk 1.87). Thus the label has the warning: “Evenity® should not be initiated in patients who have had a myocardial infarction or stroke in the preceding year.” Since there were only 41 events in the romosozumab treated patients, risk factors that might predict who would be likely to develop a MACE could not be identified.
STRUCTURE compared patients previously treated with an oral bisphosphonate who were transitioned to either romosozumab or teriparatide.3 Bone density increases in the spine and hip were greater with romosozumab (lumbar spine 9.8% vs 5.4%). Areal bone mass by CT scan was significantly greater in romosozumab-treated patients. Finite element analysis (FEA) in hips — a measure of strength — increased with romosozumab and declined with teriparatide.
The foundational effect on using romosozumab is shown by analysis of fractures in year two of the FRAME and ARCH studies. All patients in year two of FRAME were on denosumab. The increase in bone mass in year two was the same as in patients who had been on romosozumab or placebo in year one, yet the risk reduction for vertebral fracture in year two was 0.19 (81%). The increase in bone mineral density in FRAME was 13.1% at 12 months, which is equivalent to the increase in bone mass after 4.5 years of treatment with the most potent antiresorptive agent, denosumab.
Advertisement
There are no guidelines, and the following list is based on expert recommendation only:
Advertisement
Dr. Deal is Head of the Center for Osteoporosis and Metabolic Bone Disease.
Advertisement
Advertisement

A conversation with Leonard Calabrese, DO

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.