Five-year data demonstrate convergence of outcomes from years 1 to 5
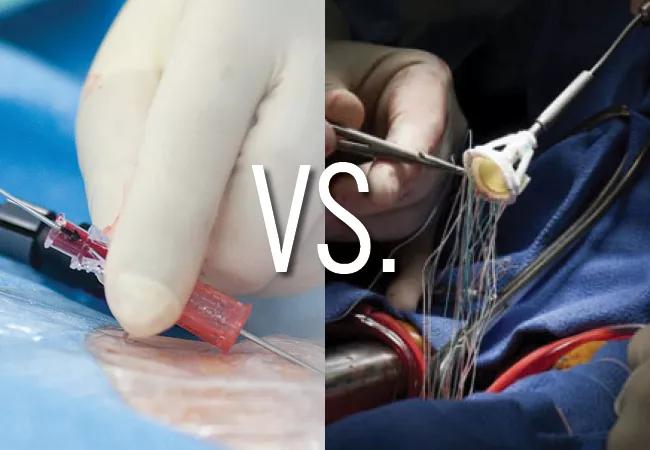
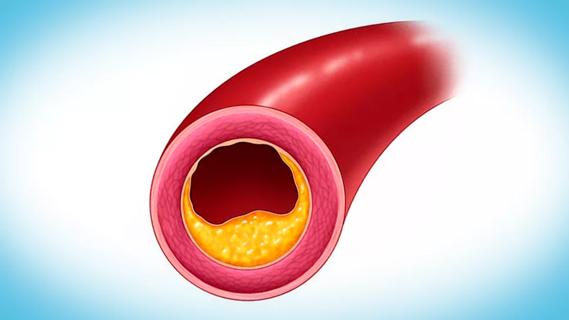
Extended follow-up data from the landmark PARTNER 3 trial comparing transcatheter and surgical aortic valve replacement (TAVR and SAVR, respectively) in patients at low surgical risk showed statistically comparable rates of a composite of death, stroke or rehospitalization — and of the individual component events — at five years.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The results, presented in a late-breaking clinical trials session at the Transcatheter Cardiovascular Therapeutics (TCT) meeting and simultaneously published online in the New England Journal of Medicine, represent an attenuation of the differences observed after one year of follow-up, which had favored TAVR.
“Previous randomized trials have shown similar five-year outcomes for TAVR and SAVR among high-risk and intermediate-risk patients, but comparative outcomes beyond two years in low-risk patients had not been reported,” says study co-author Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic. “Because low-risk patients tend to be younger than high- and intermediate-risk patients, longer-term outcomes are particularly important to clinical decision-making in this group.”
Rates of bioprosthetic valve failure were also highly comparable between the two treatment arms at five years.
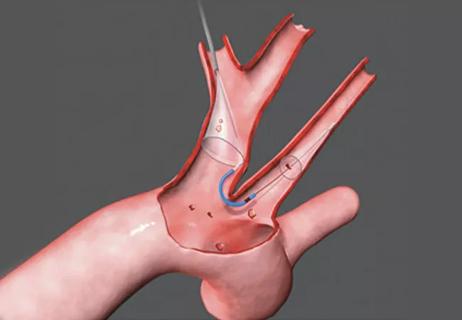
The design of the multicenter, randomized, controlled PARTNER 3 trial has been previously reported. Briefly, 1,000 patients with severe symptomatic aortic stenosis and low surgical risk were randomized 1:1 to TAVR (with the balloon-expandable Sapien 3 valve) or SAVR. For the five-year follow-up, two co-primary endpoints were prespecified:
Advertisement
“The hierarchical composite endpoint was added to better reflect the reality that some patients will experience more than one component of the composite endpoint or more than one rehospitalization over the five-year follow-up,” Dr. Kapadia explains. This second co-primary endpoint was tested using the win ratio method.
Clinical endpoint analyses used the as-treated population of 496 patients in the TAVR arm and 454 patients in the SAVR arm. Five-year follow-up was available in 94.6% of patients in the TAVR arm and 88.3% in the SAVR arm.
A vital-status sweep was performed to determine “dead or alive” status for 66 of the 95 patients who withdrew or were lost to follow-up — 21 in the TAVR group, 45 in the SAVR group. This allowed vital status to be identified for 98.0% of patients assigned to TAVR and 97.1% of those assigned to SAVR. “The vital-status sweep used here is unique and unprecedented in a trial like this,” Dr. Kapadia notes.
Kaplan-Meier event rates for the nonhierarchical co-primary endpoint (composite of death, stroke and rehospitalization) were 22.8% in the TAVR arm and 27.2% in the SAVR arm (hazard ratio [HR] = 0.79; 95% CI, 0.61-1.02; P = 0.07). This statistically similar result was maintained across all major patient subgroups.
The win ratio for the hierarchical co-primary endpoint (composite of death, disabling stroke, nondisabling stroke and rehospitalization days) was 1.17 in favor of TAVR, but not to a significant degree (95% CI, 0.90-1.51; P = 0.25).
Kaplan-Meier event rates for individual components of the composite endpoints were as follows:
Advertisement
The relative increase in mortality at five years in the TAVR arm was due to disproportionately more noncardiovascular deaths in this group, the investigators noted.
Valves’ hemodynamic performance at five years was nearly indistinguishable between the groups, with mean valve gradients of 12.8 mmHg in the TAVR arm versus 11.7 mmHg in the SAVR arm. Rates of bioprosthetic valve failure at five years were 3.3% and 3.8%, respectively.
“This similar valve durability so far is encouraging,” Dr. Kapadia says, “but we need to see whether it extends out to 10 years, given how important this factor is for the generally younger low-risk patient group.”
Functional and quality-of-life outcomes were highly comparable between the groups at five years. Rates of atrial fibrillation and bleeding were lower in the TAVR arm, while rates of paravalvular aortic regurgitation, pacemaker implantation and valve thrombosis were lower in the SAVR arm.
The latter endpoint — valve thrombosis — was the only one that differed significantly between the arms, occurring in 2.5% of the TAVR group versus 0.2% of the SAVR group (HR = 10.52; 95% CI, 1.37-80.93). The investigators note that the reasons for a higher rate of valve thrombosis with TAVR were unclear but that this did no appear to impact five-year valve durability.
“The main takeaway from these five-year results is that the two treatment strategies were equal on the primary endpoints and other outcomes of high interest, such as death, stroke and valve degeneration,” says Dr. Kapadia. “However, this is still considered intermediate-term follow-up, especially for patients at low surgical risk. Follow-up will continue out to 10 years, which will provide important insights into comparative durability of surgical and TAVR valves.”
Advertisement
“The PARTNER 3 trial has shown similar outcomes for TAVR versus SAVR except for valve thrombosis and maybe the risk of death,” adds cardiothoracic surgeon Lars Svensson, MD, PhD, Chief of Cleveland Clinic’s Heart, Vascular & Thoracic Institute. “The newly published report on five-year results particularly delved into the outcomes between one and five years after the procedure and showed hazard ratios favoring SAVR in many areas, such as death. For death, survival was initially better with TAVR at one year, but not significantly so, and now after three years, the Kaplan-Meier curves have crossed and survival is better with SAVR. While a restricted mean analysis was done for the combined endpoints ― a method for analysis when curves cross ― this was not reported for death, and later studies will need to drill deeper into the meaning and consequences of the curves for death crossing. For SAVR studies of long-term valve durability, degradation of valves is usually not expected until eight to 10 years after surgery, so the 10-year data from this trial will be of interest, not only for survival, but also to see if there are any consequences of the elevated valve thrombosis with TAVR.”
Advertisement
Advertisement

TVT Registry analysis could expand indication to lower surgical risk levels

Patient series and bench validation support efficacy and safety of CLEVE procedure

In the wake of NOTION-3 findings, a strong argument for physician judgment remains
Post hoc analysis of PROTECTED TAVR finds reduced stroke risk in the U.S. but not beyond

Analysis of STS/ACC TVT Registry finds greatest benefit in patients with prior stroke

TAVR explant demands multidisciplinary expertise

How our HVTI Advisory Services team facilitated swift improvements for an allied health organization
Support for a TAVR-first approach in patients with concurrent valve and coronary disease