Lower success rates, more hospital MACE seen with poor-quality distal targets
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a2e254d2-a7e7-44f6-b412-0a6667f4c26e/23-HVI-4078311_chronic-total-occlusion_650x450_jpg)
23-HVI-4078311_chronic-total-occlusion_650x450
In patients undergoing percutaneous coronary intervention (PCI) for chronic total occlusion (CTO), poor quality of the distal target vessel is independently associated with worse outcomes, according to a new multicenter retrospective analysis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The findings, from the largest study to date of CTO PCI outcomes in lesions with a poor-quality distal vessel, suggest that target vessel quality should be a key consideration for cardiologists when planning and performing the procedure.
“Even with all the advanced techniques we have to successfully cross a difficult occlusion in a coronary artery, if the vessel itself is not high quality, there is a higher risk of complication,” says study co-author Jaikirshan Khatri, MD, an interventional cardiologist at Cleveland Clinic. “Knowing this can help clinicians better counsel patients who are referred for these procedures so they can make better-informed decisions.”
The findings, published in JACC: Cardiovascular Interventions (2023;16:1490-1500), are based on data from 10,028 CTO PCIs performed at 39 U.S. and non-U.S. centers, including Cleveland Clinic. The information was recorded in the PROGRESS-CTO database between 2012 and 2022.
While distal vessel quality is an important variable in hybrid and global CTO crossing algorithms, most scores for CTO do not include poor distal vessel quality, and few reports exist about its impact on CTO PCI techniques and outcomes. “This study aimed to help fill that gap,” Dr. Khatri notes.
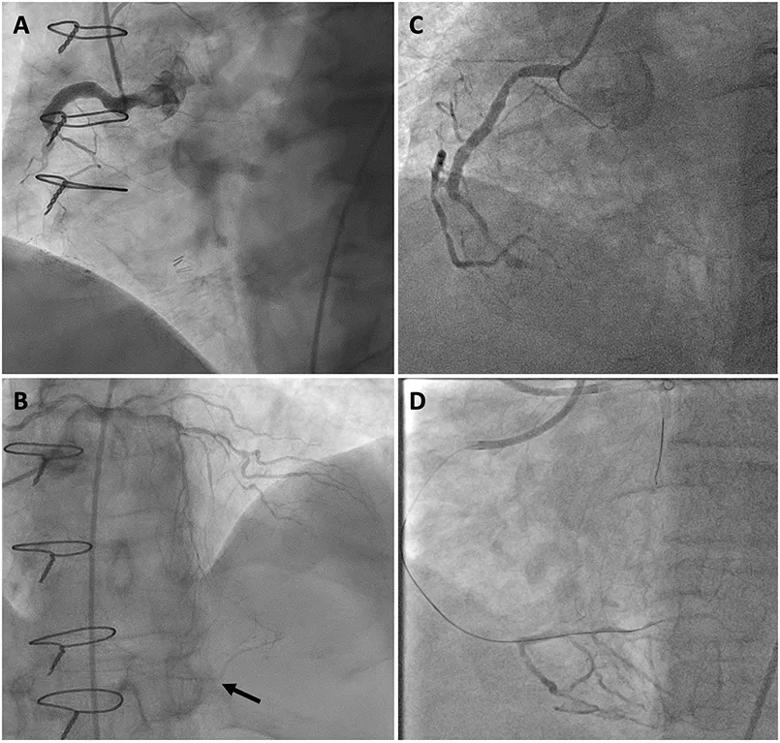
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/52e46ee2-3dd0-4cee-b562-351383a563f5/23-HVI-4078311_chronic-total-occlusion_Inset_jpg)
Figure. Images contrasting poor-quality (left) and high-quality (right) distal target vessels. Panel A shows proximal right coronary artery (RCA) chronic total occlusion (CTO). Panel B shows faint reconstitution of the distal RCA via collaterals supplied by the left coronary artery (arrow). Panel C shows proximal RCA CTO. Panel D shows robust reconstitution of the distal RCA via collaterals supplied by the left coronary artery used to direct a guide wire across the CTO.
The researchers defined CTO as a coronary lesion with a Thrombolysis in Myocardial Infarction (TIMI) flow grade 0 for at least three months’ duration. They considered a poor-quality distal vessel to have a diameter < 2 mm or significant diffuse atherosclerotic disease.
Advertisement
Technical success was defined as successful CTO revascularization achieving < 30% residual diameter stenosis within the treated segment and restoration of antegrade TIMI flow grade 3. Procedural success was defined as technical success plus the absence of major adverse cardiac events (MACE) during hospitalization. MACE included death, myocardial infarction (MI), urgent repeat target vessel revascularization, tamponade requiring pericardiocentesis or surgery, and stroke. Univariable logistic regression was used to assess variables associated with technical success and MACE.
One-third of the CTO lesions studied (3,338) were found to have a poor-quality distal vessel. Clinical characteristics associated with such vessels included a history of PCI or coronary artery bypass graft, diabetes mellitus, hypertension, dyslipidemia, prior MI, cerebrovascular disease, congestive heart failure, peripheral artery disease and slightly lower left ventricular ejection fraction.
The right coronary artery was the CTO target vessel in more than half of patients in the overall study cohort (52.8%).
Compared with CTO lesions having good-quality distal target vessels, those with poor-quality distal vessels had significantly higher Japanese CTO scores (2.7 ± 1.1 vs. 2.2 ± 1.3; P < 0.01), lower rates of technical and procedural success (79.9% vs 86.9% and 78.0% vs. 86.8%, respectively; both P < 0.01) and higher incidences of MACE and perforation (2.5% vs. 1.7% and 6.4% vs 3.7%, respectively; both P < 0.01). Poor-quality distal target vessels also were associated with trends toward higher mortality and a higher incidence of cardiac tamponade.
Advertisement
Notably, poor-quality distal vessels were associated with greater lesion complexity and with higher use of the retrograde approach for successful CTO lesion crossing (25.2% vs. 14.9%) and lower use of antegrade wiring (48.3% vs. 59.9%) and antegrade dissection and reentry (10.6% vs. 13.6%) (P < 0.01). The researchers hypothesize that the lower success rates for antegrade wiring and antegrade dissection and reentry may be due to the prevalence of calcification in poor-quality distal vessels.
CTO lesions with poor-quality distal vessels also were associated with longer procedure time (P < 0.01) and higher radiation dose (P = 0.02).
“These findings corroborate what we intuitively understood, which is that patients with poor target vessels are likely to be more challenging to care for,” Dr. Khatri observes. “The benefit of having this type of information is that it helps clinicians be much more discerning in terms of who we select for CTO PCI.”
“The data from this very impressive effort by the PROGRESS-CTO investigators indicate that the quality of the distal target is a marker of more severe and advanced disease,” notes Cleveland Clinic interventional cardiologist Khaled Ziada, MD, who was not involved in the analysis. “Lesion complexity was higher with poor-quality distal vessels, and operators more often resorted to the more complex retrograde approaches. The procedural success rate was lower, and complications were higher. To the credit of the operators’ experience, the major adverse event rate in this group was low, at 2.5%, but it’s important to recognize that the mortality rate was higher, even though the absolute numbers were low. This may have been related to serious complications, such as perforation and donor vessel injury. As the investigators point out, this should be an important consideration when taking on these cases and informing patients of the balance of risk versus benefit.”
Advertisement
“Because we have made such impressive technological advances in complex coronary interventions over the past decade, it has become even more important to parse out which patients will truly benefit from intervention,” adds Cleveland Clinic interventional cardiologist Laura Young, MD, who was not involved in the analysis. “Just because we can do it doesn’t mean it will necessarily be beneficial for the patient. This study provides further data to help us with these clinical decisions.”
Advertisement
Advertisement
5 biggest changes according to Cleveland Clinic experts
While procedural success rates lag overall, they shine for retrograde crossing
Important additions to a novel surgical technique
Retrospective findings from an executive health program spur interest in broader studies
Growing awareness of impact leads to proliferation of procedures
A scannable recap of our latest data in these clinical areas
A reliable and reproducible alternative to conventional reimplantation and coronary unroofing
Cleveland Clinic-pioneered repair technique restores a 61-year-old to energetic activity