SCAI document focuses on technical aspects of care where clear guidance had been lacking

Every day, hundreds of patients with ST-elevation myocardial infarction (STEMI) undergo primary percutaneous coronary intervention (PCI) in hospitals nationwide. Although many of these procedures are routine, some patients will present with circumstances that a catheterization laboratory team may not have the experience or equipment to handle.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Now, interventionalists can learn how their colleagues address similar situations by turning to a new expert consensus statement from the Society for Cardiovascular Angiography and Interventions (SCAI) on the management of patients with STEMI referred for primary PCI (J Soc Cardiovasc Angiog Intervent.Epub 2024 Oct 7).The consensus statement is designed to complement existing STEMI therapy guidelines by focusing on the technical aspects of treatment.
“Our purpose is to provide direction on various aspects of care that cardiologists encounter every day in the cath lab and for which directions are often not clear,” says the statement’s lead author, Jacqueline Tamis-Holland, MD, Director for Acute Coronary Care in Cleveland Clinic’s Section of Invasive and Interventional Cardiology.
As an interventional cardiologist with a specialty interest in STEMI, Dr. Tamis-Holland noticed that colleagues described a variety of approaches to managing STEMI. In some situations there were varying perspectives on how to approach the condition, while in other circumstances there seemed to be a clear consensus. Given the different perspectives, Dr. Tamis-Holland approached the SCAI about the need for a consensus statement on best practices. Following their approval, she formed a 12-person panel of experts to tackle the subject.
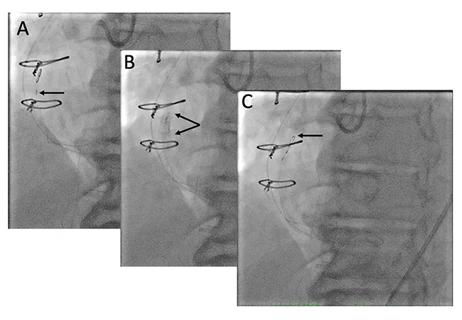
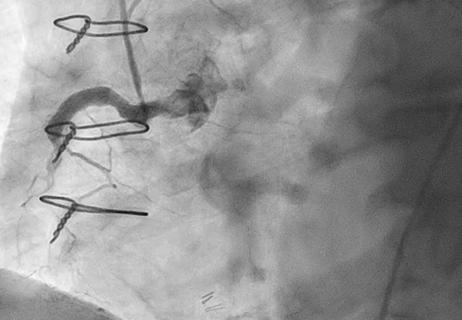
Their document highlights the strengths and limitations of diagnostic and therapeutic interventions used to access and treat STEMI in the cath lab, reviews options for managing large intracoronary thrombus during STEMI and coronary no-reflow, and lays out STEMI management options in special anatomical and clinical circumstances. In addition to outlining best practices for cath lab team readiness, the statement includes an algorithm for determining proper arterial access in STEMI and explores questions around the timing of diagnostic angiography.
Advertisement
“Most discussions in the document center on various ways you can approach a problem,” Dr. Tamis-Holland says. “Sometimes we came away with a consensus that it is ‘best’ to do it in a consistent way, while other times we laid out a given situation and identified conditions when one approach makes sense and other conditions when a different approach is best.”
Dr. Tamis-Holland says several important messages surfaced as the team developed the consensus statement, including:
The writing process also revealed areas where additional research is needed to determine best practices. These include finding a better method for identifying patients with total occlusion and addressing reperfusion injury and no-reflow in order to reduce infarct size.
Advertisement
The consensus statement acknowledges that cath labs vary in degree of sophistication — for instance, some are not equipped for interventions on patients in advanced cardiogenic shock. Basic cath labs might recognize their limitations for stable patients but may not have an opportunity to choose to accept only the “low risk” patient with STEMI. For this reason, the statement advises, all labs should be equipped with certain tools to manage all types of patients with STEMI. After the initial PCI, they may then wish to transfer those patients needing more advanced care to more-experienced institutions.
According to Dr. Tamis-Holland, cath labs that are open around the clock are well advised to be prepared for all comers. “You can’t know who is going to present — whether it’s someone who needs support, an atherectomy device or imaging — until you see them,” she says. “It may be a patient you’re not equipped to handle and who will be transferred out, but you still need to be able to put in a device that will support them until they get to another hospital.”
The consensus statement is expected to fill a need in smaller-volume institutions and for operators without ready access to more experienced colleagues.
“If operators are treating STEMI with their usual approach and everything is going well, that’s great,” Dr. Tamis-Holland says. “But if they know only one approach and are having difficulties, this document brings to light how others have handled the situation. It’s great to hear about different ideas so we can consider all the techniques when we find ourselves in new or different situations.”
Advertisement
“This is an important document that expands on the current guidelines and provides best practices from national experts on how to provide optimal care for STEMI patients,” adds interventional cardiologist Grant Reed, MD, MSc, former director of Cleveland Clinic’s STEMI program. “It fills an important need in the interventional community, and it may help standardize operating procedures across institutions.”
Advertisement
Advertisement

In the wake of NOTION-3 findings, a strong argument for physician judgment remains

Transvalvular LVAD support transforms emergency surgery into urgent procedure

Study identifies a cohort of low-risk patients, finds LVEF predicts late VT/VF in those at higher risk
Support for a TAVR-first approach in patients with concurrent valve and coronary disease
While procedural success rates lag overall, they shine for retrograde crossing
Lower success rates, more hospital MACE seen with poor-quality distal targets

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon