Support for a TAVR-first approach in patients with concurrent valve and coronary disease
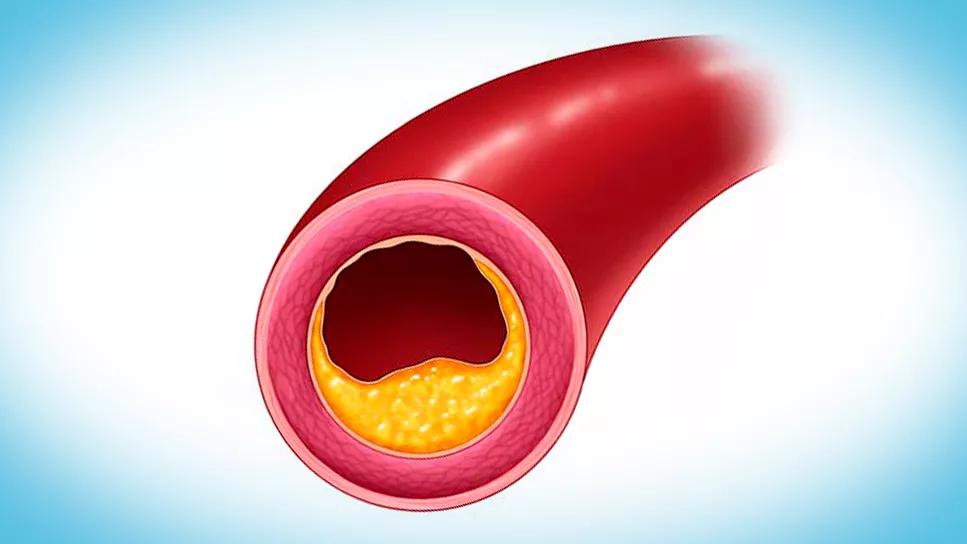
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/84a8cdc9-c3ad-423c-a610-d1b67c9a0403/atherosclerosis-in-coronary-artery)
atherosclerosis in coronary artery
In a retrospective analysis of nearly 2,000 patients undergoing transcatheter aortic valve replacement (TAVR), untreated stable obstructive coronary artery disease (CAD), even in high-risk anatomic substrates, did not increase procedural complications or portend worse longer-term outcomes relative to nonobstructive CAD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The findings, reported by Cleveland Clinic researchers in European Heart Journal (Epub 2024 Jan 25), suggest that a TAVR-first approach is a viable option in this patient population.
“Our study demonstrates the procedural safety of TAVR in patients with varying degrees of untreated stable obstructive CAD,” says corresponding author Rishi Puri, MD, PhD, an interventional cardiologist at Cleveland Clinic. “Rates of periprocedural complications were very low, and neither complications nor longer-term rates of major adverse cardiovascular events (MACE) or death differed significantly between patients with and without obstructive CAD.”
The analysis was prompted by controversy around when — or even whether — to address stable obstructive CAD in patients who need to undergo TAVR for severe aortic stenosis, which coexists with CAD in many patients.
“Delaying revascularization might render it safer when it is done in the presence of a normally functioning aortic valve,” notes co-author Amar Krishnaswamy, MD, Section Head of Invasive and Interventional Cardiology. “At the same time, accessing the coronary vessels across a bioprosthetic valve after TAVR might present challenges in some instances. We undertook this analysis to guide practice for this patient population at Cleveland Clinic, where we have tended to favor a TAVR-first approach in patients with symptoms that are likely due to valve disease alone.”
Among 2,952 patients who underwent TAVR at Cleveland Clinic between January 2015 and December 2021, 1,911 had stable CAD and made up the study cohort. Patients with acute coronary syndrome (ACS) prior to TAVR were excluded. Eligible patients were categorized into four groups based on CAD extent and severity:
Advertisement
The primary outcome measure was a composite of all-cause death, MACE (ACS, stroke or heart failure hospitalization) or unplanned coronary revascularization during follow-up. Procedural death and complications (cardiogenic shock, need for extracorporeal membrane oxygenation or intra-aortic balloon pump, or ventricular arrhythmias requiring defibrillation) were also assessed.
Across the overall study population, rates of periprocedural death (n = 7) and complications (n = 6) were low (0.7% combined incidence). No significant between-group differences in procedural death or complications were observed.
Over median follow-up of 21 months, the incidence of the composite outcome was statistically comparable between the nonobstructive and obstructive CAD groups, as were rates of all-cause mortality and MACE. These findings were maintained after multivariable analysis.
The researchers note that their findings provide reassurance on the safety of a TAVR-first approach in stable patients with concomitant obstructive CAD, challenging recent European guidelines that recommend revascularization before TAVR in high-risk anatomic scenarios.
“There was no indication that the TAVR procedure contributed to higher rates of acute coronary syndrome, death or revascularization,” Dr. Puri observes. “The rates of ACS and unplanned revascularization at one year were low and typical of the natural history and progression associated with patients’ background burden of CAD.”
“Our findings suggest that stable, obstructive CAD, even in high-risk anatomic substrates, can be managed in keeping with current CAD guidelines in TAVR candidates,” adds Dr. Krishnaswamy. “However, additional studies are needed to evaluate the optimal treatment strategy for patients with concurrent coronary and aortic valve disease.”
Advertisement
Indeed, the authors’ study report notes that guidance on this question is expected from the ongoing COMPLETE TAVR trial (Staged Complete Revascularization for Coronary Artery Disease vs Medical Management Alone in Patients With AS Undergoing Transcatheter Aortic Valve Replacement; NCT04634240). This randomized study is evaluating whether systematic post-TAVR percutaneous coronary intervention in angiographically severe lesions will influence long-term cardiovascular outcomes compared with optimal medical management.
“While our data support a TAVR-first approach in patients with stable obstructive CAD, valve choice and anatomical characteristics still have a role in an operator's decision on the need for, and timing of, percutaneous coronary intervention (PCI) in relation to TAVR,” Dr. Puri concludes.
“When a treatment plan for TAVR and PCI is chosen over surgical aortic valve replacement and coronary artery bypass grafting in a patient with significant aortic stenosis and coincident CAD, multiple issues are considered to determine the optimal sequence of TAVR and coronary intervention,” adds cardiothoracic surgeon James Yun, MD, PhD, a co-author on the study. “This analysis in a large cohort of patients adds important data that will aid multidisciplinary TAVR teams in decision-making in this context.”
Advertisement
Advertisement
TVT Registry analysis could expand indication to lower surgical risk levels
Patient series and bench validation support efficacy and safety of CLEVE procedure
In the wake of NOTION-3 findings, a strong argument for physician judgment remains
Post hoc analysis of PROTECTED TAVR finds reduced stroke risk in the U.S. but not beyond
Analysis of STS/ACC TVT Registry finds greatest benefit in patients with prior stroke
TAVR explant demands multidisciplinary expertise
How our HVTI Advisory Services team facilitated swift improvements for an allied health organization
Five-year data demonstrate convergence of outcomes from years 1 to 5