While procedural success rates lag overall, they shine for retrograde crossing
The Carlino technique for crossing chronic total occlusions (CTOs) is growing in use but still relatively infrequent, as it is largely reserved for the most complex lesions. Although its procedural and technical success rates are lower than those with other CTO percutaneous coronary interventions (PCIs), its procedural success is significantly higher when used for retrograde crossing. So concludes the largest study of the evolving Carlino technique to date, recently published in the American Journal of Cardiology (2023;207:305-313).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Interventional cardiologists are performing an increasing number of CTO PCIs, so we are all interested in novel techniques that can improve success rates for these notoriously difficult procedures,” notes Cleveland Clinic interventional cardiologist Jaikishan Khatri, MD, a co-author of the multicenter retrospective registry analysis. “This study provides valuable real-world data on Carlino use in contemporary practice, its application in complex cases and its impact on procedural success and complications.”
The Carlino technique, introduced in 2008, allows carefully controlled injection of small amounts of contrast to alter plaque compliance and enable passage of guidewires where traditional crossing attempts have failed (Figure). Small studies and case series have shown promise for bailout use of the technique in the most challenging lesions. However, data on overall utilization rates and larger-scale outcomes have been lacking.
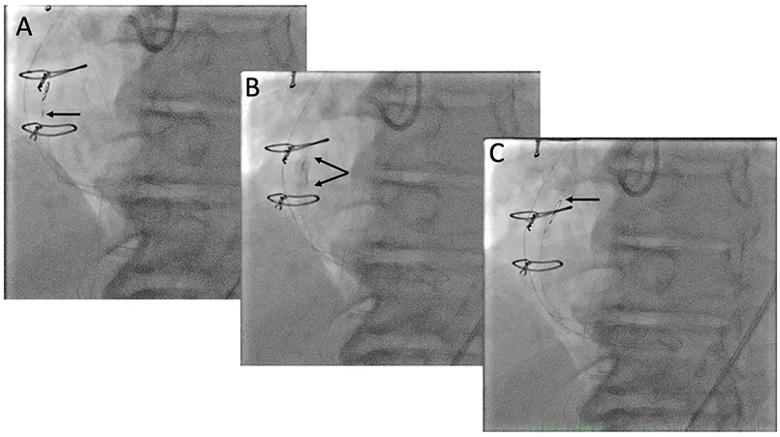
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8371763b-81ad-4883-9fa3-87ed73a9fd8c/23-HVI-4400490-CQD-Inset_jpg)
Figure. Images from a patient who underwent the Carlino technique. (A) Retrograde microcatheter (black arrow) was used to deliver a knuckle wire that failed to cross the CTO. (B) Retrograde microcatheter was wedged into the CTO distal cap and 1 mL of contrast was injected to hydraulically modify plaque compliance. (C) After the Carlino technique, retrograde knuckle wire (black arrow) was able to cross the CTO.
The new investigation analyzed data on utilization, applications and outcomes of the Carlino technique from the ongoing PROGRESS-CTO registry encompassing over 11,000 CTO PCIs from 22 U.S. and international centers from 2016 to 2023.
Of 4,508 CTO PCIs performed using antegrade dissection and reentry (78.9%) or the retrograde approach (21.1%), the Carlino technique was employed in 128 cases (2.8%). Use varied substantially among centers, from 1% to 18% of relevant cases. However, Carlino use increased progressively over the study period (P < 0.001), from 0% of cases in 2016 up to 8.3% in 2023.
Advertisement
Notably, Carlino cases had higher complexity by multiple metrics:
“These findings suggest that the Carlino technique has become an increasingly used bailout strategy for the most difficult lesions,” Dr. Khatri observes.
Cases in which the Carlino technique was used had significantly lower technical success (65.5% vs. 78.5%; P < 0.001) and procedural success (63.3% vs. 76.5%; P < 0.001) relative to the rest of the CTO PCI cases. Median procedure time (188 vs. 158 minutes), contrast dose (250 vs. 230 mL) and radiation exposure (3.6 vs. 2.6 Gy) all were significantly higher with the Carlino technique as well.
However, success varied substantially by approach. Retrograde Carlino cases had a 81.5% procedural success rate compared with 58.4% for antegrade dissection and reentry (P = 0.047).
Complication rates were higher in the Carlino group, including perforation (18.0% vs. 8.9%), need for pericardiocentesis (3.9% vs. 1.3%) and contrast-induced nephropathy (2.3% vs. 0.4%). Reassuringly, only five perforations were attributable to the Carlino technique itself.
These real-world data provide several key insights into use of the Carlino technique:
Advertisement
“When applied judiciously in appropriate cases by expert operators, the Carlino technique shows promise for improving outcomes over conventional crossing methods for CTO PCI,” Dr. Khatri says. “However, for less experienced operators, the steep learning curve with the technique and the higher risks observed here warrant caution. As larger CTO PCI registries accrue long-term data, we will learn even more about which patients stand to benefit most from the Carlino technique and when restraint is advisable.”
“Studies such as this are crucial for us to understand which specific patient populations these super-specialized techniques may potentially benefit,” adds Cleveland Clinic interventional cardiologist Laura Young, MD, who wasn’t involved in the study. “This registry suggests that the Carlino technique may be particularly helpful in patients with more technically difficult CTOs, where our conventional wiring strategies have failed.”
Advertisement
Advertisement
5 biggest changes according to Cleveland Clinic experts
Lower success rates, more hospital MACE seen with poor-quality distal targets
Important additions to a novel surgical technique
Retrospective findings from an executive health program spur interest in broader studies
Growing awareness of impact leads to proliferation of procedures
A reliable and reproducible alternative to conventional reimplantation and coronary unroofing
Cleveland Clinic-pioneered repair technique restores a 61-year-old to energetic activity
In the wake of NOTION-3 findings, a strong argument for physician judgment remains