While mortality was unaffected, later surgery was associated with more reoperations
Despite guideline recommendations favoring early surgery in patients with severe degenerative mitral regurgitation (MR), rates of early surgical referral for degenerative MR to a high-volume valve center remain modest. So finds a new retrospective analysis from Cleveland Clinic. Timing of surgical referral had no effect on survival, but later referral correlated with more reoperations.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In a recent five-year period, nearly three-quarters of the patients in whom we performed primary isolated mitral valve surgery already had symptoms, left ventricular dysfunction, atrial fibrillation or pulmonary hypertension,” says Cleveland Clinic cardiothoracic surgeon Daniel Burns, MD. “Rates of in-hospital and mid-term mortality were similar between the early- and late-surgery groups, but later surgery was associated with more reintervention procedures.”
Dr. Burns was a co-author of the study, which was presented at the 70th annual meeting of the Southern Thoracic Surgical Association in Orlando, Florida.
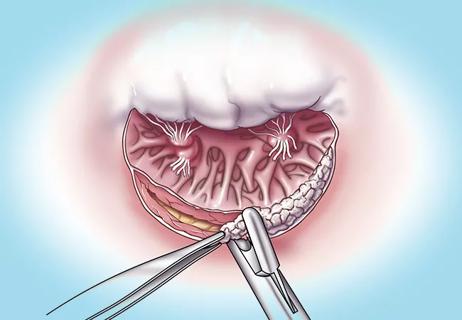
The thresholds for surgical intervention in degenerative MR have gotten lower and lower as surgical procedures for mitral valve repair have become more durable and less risky. This trend is reflected in the 2020 American College of Cardiology/American Heart Association guideline on valvular heart disease, which states that early surgical repair is reasonable for patients with severe primary MR caused by degenerative mitral valve disease even if they are asymptomatic and have normal left ventricular systolic function — specifically when repair can be performed at a primary or comprehensive valve center.
“Evidence from the literature shows that patients who undergo surgery for mitral regurgitation after they already have significant ventricular dysfunction do not fare as well,” Dr. Burns observes. “In this study, we sought to define trends in the timing of surgery for degenerative MR and assess the effect of early surgery on in-hospital and mid-term outcomes.”
Advertisement
He and colleagues analyzed primary isolated mitral valve surgeries for degenerative MR performed at Cleveland Clinic between January 2016 and July 2020, identifying 1,824 adults who underwent such a procedure.
Using propensity matching, they compared rates of in-hospital complications, operative mortality, mid-term survival and freedom from reoperation according to whether patients underwent early or late surgery. Early surgery was defined as a procedure performed before onset of any of the following:
Overall, 492 of the MR surgeries during the study period were performed early (27%) and 1,332 were performed late (73%). Notably, the proportion of overall surgeries that were early procedures remained constant throughout the study.
“We were surprised that the share of early surgeries didn’t increase over time,” Dr. Burns notes. “In some cases, delays in surgery may have been because patients were reluctant to have surgery at their local institution. On average, cardiac surgeons in the U.S. perform five to 10 mitral valve repairs per year. Our surgeons average 80 or more of these procedures per year, which contributes to our high success rates,” which include 0% mortality for all isolated mitral valve repairs dating back to 2014.
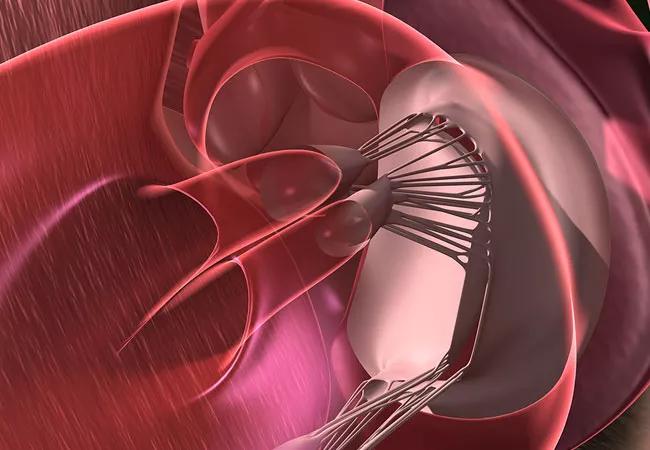
Mitral valve repair was accomplished in almost all cases across the cohort, although the rate of repair was higher in the early surgery group (99.6% of cases) than in the late surgery group (96.2%) (P < 0.001). Minimally invasive robotically assisted repair was used more often in the early group than the late group (54% vs. 29%; P < 0.001).
Advertisement
With propensity matching, the authors identified 485 matched pairs (99% of possible matches). Among matched patients, there were no in-hospital deaths and rates of major in-hospital morbidity were similar between the early and late surgery groups (3.8% vs. 4.6%, respectively; P = 0.5).
At median follow-up of 3.5 years, there were 11 deaths (4 in the early group, 7 in the late group) and 28 patients in the matched cohort had undergone mitral valve reoperations — 8 in the early group and 20 in the late group. Overall survival rates were 99.8%, 99% and 98% at 1, 3 and 5 years, respectively, with no significant differences between the early and late groups. However, patients who underwent late surgery were more likely to have a subsequent reoperation (P = 0.02).
Dr. Burns says that reasons for the increased rate of reoperation in the late surgery group are uncertain but “it could be that remodeling of the heart that had already begun in these patients led to a need for procedures on other cardiac structures.”
The key question the researchers would like to address in future studies is how long is too long to wait for MR repair, Dr. Burns notes. They also plan to examine the impact of late surgery on functional status, heart rhythm, left ventricular function and long-term survival.
“It’s important to keep in mind that hospitalization, reintervention and mortality are only part of the picture for these patients,” he adds. “Quality of life and cardiac function play a more long-term role. We did not formally examine these measures, but they are likely influenced by delays in surgery.”
Advertisement
When asked about the main clinical takeaway from the current study, Dr. Burns says: “Patients with severe degenerative MR stand to benefit from surgical repair regardless of when they are referred, particularly if they are treated at a high-volume center of excellence for valve procedures.”
At the same time, the Cleveland Clinic team urges early referral whenever possible. “Degenerative MR should be followed closely and referred for consultation early, prior to development of significant symptomatology, left ventricular dysfunction or dilatation,” says cardiothoracic surgeon Tarek Malas, MD, who wasn’t involved in the study. “Late referral also may preclude treatment modalities that employ minimally invasive surgery. We strongly encourage early conversation between family physicians, cardiologists and cardiothoracic surgeons to optimize timing of intervention in these patients.”
“Degenerative mitral regurgitation can lead to various long-term complications, such as atrial fibrillation, heart failure and pulmonary hypertension,” adds Cleveland Clinic cardiologist Serge Harb, MD. “This study underscores that early surgery, before the onset of overt complications, is associated with increased use of minimally invasive approaches and a higher likelihood of a durable repair. Reassuringly, even in the group of patients who ended up having delayed surgery, outcomes remained excellent at this high-volume center.”
Advertisement
Advertisement

Optimal management requires an experienced center

Multimodal evaluations reveal more anatomic details to inform treatment

Provides option for patients previously deemed anatomically unsuitable
Surgical tips on debridement of calcification to optimize valve replacement
Superiority continues even after significant crossovers from control group at 2 years

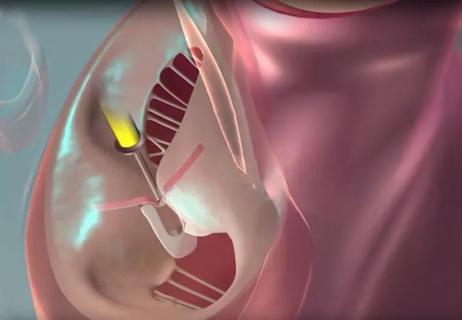
How Cleveland Clinic is using and testing TMVR systems and approaches

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic