Multidisciplinary teams can deliver good short- and long-term outcomes, Cleveland Clinic experience shows
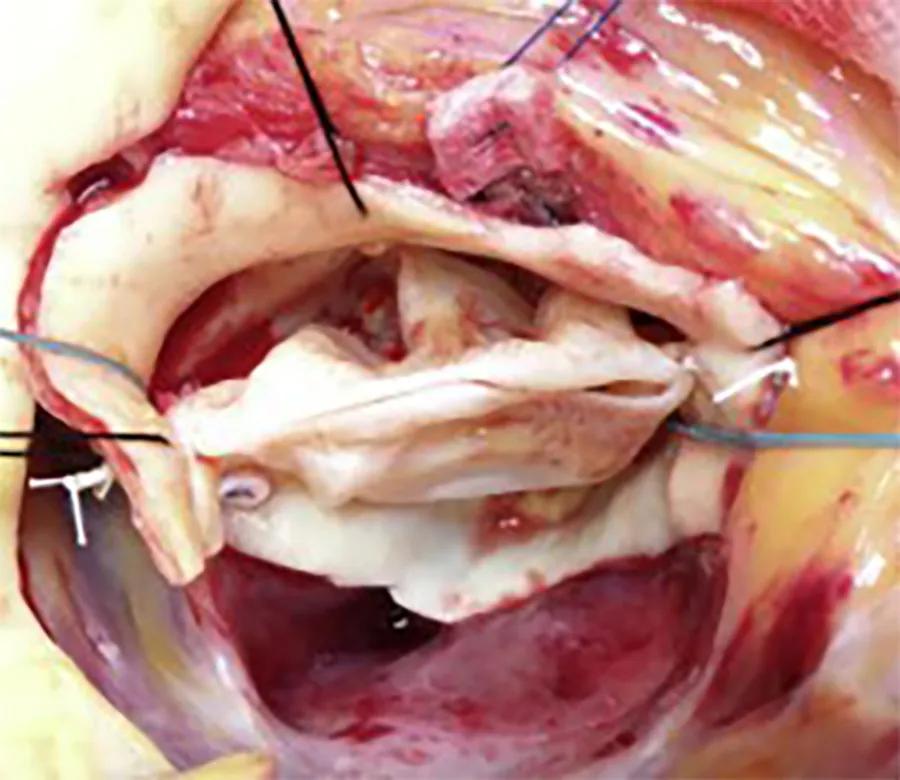
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3d12d2ea-144a-4baa-832f-e45b1eab0db2/Bicuspid-AV-dilated-ascending-aorta-featute)
intraoperative photo of a bicuspid valve repair operation
In most cases, a bicuspid aortic valve (BAV) can be surgically treated very safely and effectively — with or without root replacement — even for severe regurgitation and accompanying aortic dilation and aneurysm. Indeed, most patients with severe regurgitation can have a successful repair. Surgeon experience is critical to success for these complex operations, as is careful assessment to determine patient candidacy and appropriate operative strategy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“For the past 40 years, Cleveland Clinic surgeons have pioneered BAV repair techniques for patients with BAV regurgitation, gaining considerable expertise and longitudinal data on patient outcomes,” says Xiaoying Lou, MD, a Cleveland Clinic cardiothoracic surgeon with specialty interests in the aorta and aortic valve. “In the current era, repair can be just as good as replacement: Our 10-year survival rate for elective BAV repair is 95%, with a 0.7% combined incidence of operative mortality and stroke.”
A BAV occurs in about 1% to 2% of the population and may be associated with an inherited connective tissue disorder. Many of these patients develop valvular regurgitation that requires intervention. Patients with a BAV are prone to progressive problems — including aortic regurgitation, stenosis and aneurysms — starting decades earlier than for patients with a tricuspid aortic valve. In the Cleveland Clinic experience, more than one-third develop aortic enlargement.
When possible, experienced surgeons prefer to perform repair over replacement for younger patients with a tricuspid aortic valve and a dilated root, to avoid prosthetic valve complications and lifelong anticoagulation therapy. However, BAV repair poses additional challenges that many surgeons are reluctant to take on, especially in centers where BAVs are not encountered often.
For aortic stenosis in patients with a BAV, the strategy is generally to surgically replace the valve, except in specific circumstances where the valve is also regurgitant and the leaflets are of sufficient quality to enable repair. Dr. Lou considers transcatheter aortic valve replacement (TAVR) in the setting of BAV only for older patients who are unable to undergo surgery due to comorbidity, as bicuspid anatomy is not conducive to good placement of the TAVR valve and the risk of stroke and paravalvular leaks is higher.
Advertisement
“We don’t offer TAVR even for a medium-risk patient with a BAV,” she says. “If the valves are calcified, as they often are, the patient might end up with a worse leak and poor options for a future fix.”
“Aortic regurgitation is a difficult valve lesion to assess, because it is easy to underestimate the severity of the leak and its impact on left ventricular function,” says Brian Griffin, MD, Medical Director of Cleveland Clinic’s Valve Center. “Imaging plays a large role in preoperative assessment, as it provides important clues for determining timing of intervention, which is especially critical for asymptomatic patients.”
He adds that unlike for the mitral valve, aortic valve intervention is unlikely to last a lifetime in younger patients like those with a BAV, so delaying it until really needed can be beneficial. On the other hand, if one waits until the left ventricle has become enlarged and function is compromised, it may not improve after an intervention. Another consideration is that for women, intervention generally should be undertaken earlier than guidelines often indicate, as women’s hearts tend to be smaller than men’s and appear to have greater difficulty handling an aortic leak.
Dr. Griffin co-authored a paper in JACC: Cardiovascular Imaging (2018;11[10]:1499-1513) outlining Cleveland Clinic’s strategy for determining whether a patient with chronic asymptomatic aortic regurgitation should be considered for surgery. Severity of aortic regurgitation and left ventricular function are the primary initial considerations, including in patients with BAV. Patients with aortic regurgitation should be monitored with echocardiography to track changes in left ventricular size and volume. Every one to two years, stress echocardiography should be done to objectively assess functional capacity. If results are unclear, MRI can provide quantitative measures of ventricular size and aortic regurgitation severity.
Advertisement
“We use multiple imaging modalities if needed, particularly in patients with a bicuspid valve, but there is no textbook answer in determining optimal timing for intervention,” Dr. Griffin explains. “Experience is critical.”
Once surgery is decided on, issues surrounding replacement versus repair become paramount. The decision is based on patient age (repair is especially advantageous for younger patients) and preoperative and intraoperative clinical findings. Replacement is needed for patients with moderate to severe aortic stenosis.
Patients with a preoperative aortic root or ascending aorta diameter of more than 4.5 cm, or who have an aortic area-to-height ratio of more than 10, are candidates for replacement of the ascending aorta in addition to valve repair or replacement.
Systematic intraoperative assessment of commissures, leaflets, anulus, sinuses and sinutubular junction (CLASS) helps determine strategy and techniques. For patients with heavy calcification or major perforations of valve leaflets, replacement is recommended.
Dr. Lou emphasizes the imperative to ensure that results are optimal — with good function and no leakage, as determined visually and with intraoperative echocardiography — before closing the incision.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f35d38ea-d4f1-401c-8bdf-5b3859885d66/Bicuspid-AV-dilated-ascending-aorta-inset)
Figure. Intraoperative photographs of BAV repairs using Cabrol sutures, plication stitches and figure-of-8 sutures. Note the suture placement near the leaflet edge and the use of a Hegar dilator to ensure that stenosis is not created. Reprinted under the CC BY-NC-ND license from Svensson LG, “The art of aortic valve repair,” JTCVS Techniques. 2021;7:121-125. ©2021 The Authors.
A study comparing Cleveland Clinic patients who underwent aortic root replacement with either BAV reimplantation (n = 92) or tricuspid aortic valve reimplantation (n = 515) from 2002 to 2017 found similar short-term and five-year outcomes among 71 matched pairs (J Thorac Cardiovasc Surg. 2022;163[1]:51-63). However, higher gradients, less ventricular reverse remodeling and more aortic valve reoperations in the BAV group indicated a need for continued surveillance in such patients.
Advertisement
Another Cleveland Clinic study analyzed more than two decades of data (1998-2020) from patients who underwent BAV repair with (n = 419) or without (n = 421) ascending aorta replacement (J Thorac Cardiovasc Surg. 2023;166[6]:1561-1571). Between-group comparisons were made among 97 patient pairs after propensity score matching.
At 10 years, across the overall cohort, survival was 95% after BAV repair with aorta replacement and 96% after BAV repair alone, and rates of freedom from reoperation were 79% and 75%, respectively. Among the matched pairs, severe aortic regurgitation developed within 10 years in 9.1% of patients undergoing BAV repair alone and 11% of those with BAV repair plus aorta replacement (P = .33). Among other findings:
Dr. Lou notes that an important focus of the study was to determine the importance of replacing the ascending aorta with a tube graft for the sole purpose of stabilizing the sinutubular junction (STJ). BAV is often seen with ascending aortic aneurysms leading to STJ effacement, disrupting optimal commissural alignment and resulting in aortic regurgitation. However, comparison of the matched pairs revealed that stabilization of the STJ with ascending aorta replacement at the time of BAV repair had minimal effect on long-term repair durability. The authors concluded that STJ stabilization should not be undertaken solely for that purpose.
Advertisement
Both Drs. Lou and Griffin emphasize that with the number of considerations surrounding surgery for BAV disease, decisions are best made with the input of the full heart care team. “We all need to be on the same page regarding what a patient needs and what can realistically be accomplished,” Dr. Lou says.
“A patient’s lifestyle, hopes and expectations are also critically important,” Dr. Griffin adds. “There’s no single recipe for a correct solution in these complex situations.”
Advertisement
Indication, timing and options for surgical intervention
Join us in New York City Dec. 5-6
30-year study of Cleveland Clinic experience shows clear improvement from year 2000 onward
Study examines data and clinical implications for performing Ross procedures in infancy versus later in life
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Choice between smaller or larger prosthesis is a tradeoff between leak and pacemaker risks
4-D imaging informs complex aortic valve repair in adult and pediatric patients
Study offers guidance on an increasingly common presentation