Improving safety, efficacy and access for emerging therapies
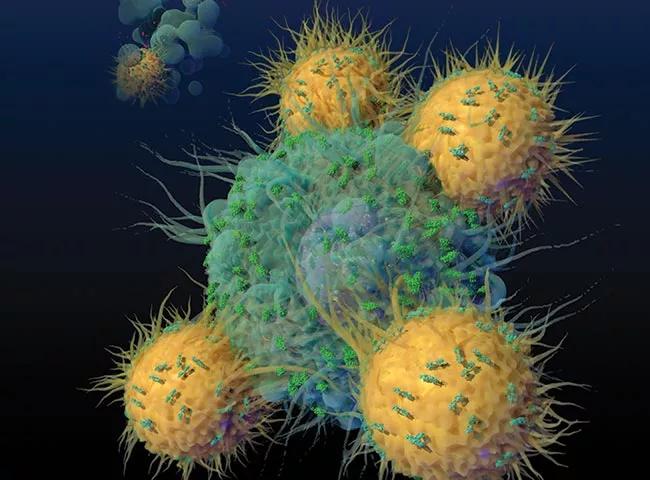
Chimeric antigen receptor (CAR) T-cell therapy has profoundly changed the treatment landscape, bringing the promise of durable remission for many patients with blood cancers. This specialized therapy involves genetically modifying a patient’s own T cells and infusing them back into the bloodstream so they can recognize and eradicate cancer cells. This has brought hope to patients with relapsed or refractory disease such as large B-cell lymphoma and acute lymphoblastic leukemia (ALL).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Yet confounding questions remain about this emerging treatment: Why does it cure some patients and fail in others? What can we do to increase access to these therapies? And how can we get treatment to those who simply cannot wait the weeks it currently takes to manufacture T cells?
Researchers like J. Joseph Melenhorst, PhD are working to unravel these mysteries. Recently recruited to Cleveland Clinic from the University of Pennsylvania, where he was instrumental in bringing CAR T-cell therapy into patient care, he is on a quest to broaden the scope of what’s possible with this treatment.
As the Director of the new Cell Therapy and Immuno-Engineering Program and Vice Chair of the Center for Immunotherapy and Precision Immuno-Oncology at Cleveland Clinic, Dr. Melenhorst is leading research into the clinical efficacy of CAR-engineered NK and T cells. “Providing access to effective CAR-based therapies for those with aggressive disease is a particular challenge,” he says. “There is much work to be done in understanding how we can fine-tune the manufacturing process. Off-the-shelf CAR products that are T-cell or NK-cell based are one means to accelerate treatment.”
Researchers at the Center for Immunotherapy and Precision Immuno-Oncology are investigating ways to make CAR T-cell therapy more effective. In many cases, this involves evaluating multiple targets. “Particularly in pediatric ALL, we have seen relapse occurring when the tumor has lost expression of the biomarker CD19,” says Dr. Melenhorst. “This has led to novel CAR designs where dual targeting or even triple targeting of CD19, CD20 or CD22 is included. Hopefully this approach will bring sustained remissions for patients, even if they lose CD19 expression.”
Advertisement
In addition to improving efficacy, researchers are seeking safer ways to deliver CAR T-cell therapy.
A key challenge that has stymied clinicians is how to manage the side effects of CAR T-cell therapy. After cell infusion, immune system cells can become overly stimulated and cause cytokine release syndrome (CRS). This may lead to fever, labored breathing or temporary neurological issues. Researchers are pursuing several avenues for minimizing these adverse events.
Identifying IL-6 as a potential target using monoclonal antibodies such as tocilizumab was one of the first clinical breakthroughs for controlling CRS. Researchers are also beginning to use predictive modeling to develop diagnostic tests for early intervention. By carefully analyzing cytokine secretion profiles early after infusion, they can forecast severe CRS. “Ultimately, the goal is to understand and manage CRS by preventing it from happening,” says Dr. Melenhorst.
Another area of interest for Cleveland Clinic is how to increase access to CAR T-cell therapies. Currently, these treatments are only accessible through specialized centers, which can be a major obstacle for some patients. “Developing CAR-based treatments that can be delivered as outpatient therapies will make these options more accessible and more affordable,” says Dr. Melenhorst. “I think the therapies we’re evaluating here will allow us to get to the point where we don’t have to hospitalize patients for CAR T-cell therapy anymore.”
Dr. Melenhorst recently co-authored a study demonstrating sustained remission in two patients with chronic lymphocytic leukemia a decade after CAR T-cell infusion. He and his colleagues soon received handwritten letters from patients who were excited by the study and who wanted a cure for their cancer. “It was a sobering reminder that so much work still needs to be done,” he says.
Advertisement
His team is now collaborating with researchers at Case Western Reserve University as well as other institutions in the U.S. and abroad to improve our understanding of CAR T-cell therapies. “Cleveland Clinic has made a major commitment to developing immunotherapies for cancer, and working together with many others, we are inching closer to predictive modeling of the efficacy of therapies that we develop and administer to patients,” he says. “I believe we’ll arrive at a point where we can offer patients multiple treatment options that induce durable remissions.”
Hear our podcast with Dr. Melenhorst about the future of CAR T-cell therapy.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient