Limited data and experience will translate to a cautious rollout
Recent FDA approval of the first two devices for transcatheter treatment of tricuspid valve regurgitation marks an important step toward access to new treatment strategies for a patient population with few other options. But because both devices were approved under the FDA’s breakthrough device designation, their path to coverage by the Centers for Medicare & Medicaid Services (CMS) will likely require cautious rollout and accrual of supportive postmarket evidence.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“These approvals in the breakthrough device category are a bit of a new development for the structural cardiology community,” says Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic, who has been involved in clinical testing of both new tricuspid valve devices. “Because the initial data are more limited than is typically the case, CMS will be taking particular care to ensure these devices will be used in the right patients in the right way by the right operators and facilities. And patients are well advised to seek care with these devices from centers that are experienced in their use and can offer a full heart team approach to tricuspid valve disease.”
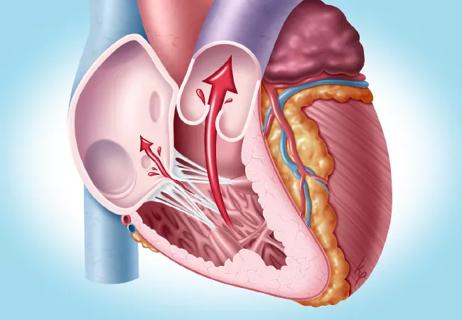
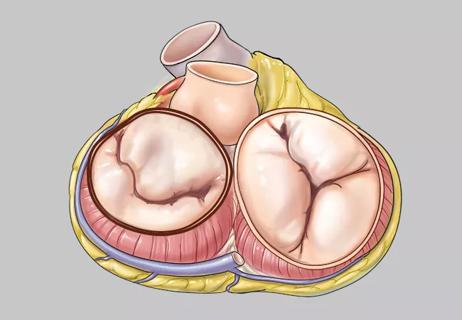
The two new devices — the Evoque transcatheter tricuspid valve replacement system from Edwards Lifesciences and the TriClip™ transcatheter edge-to-edge repair (TEER) system from Abbott — represent novel and minimally invasive approaches to the treatment of tricuspid regurgitation (TR).
TR can lead to right-sided heart failure and is well recognized for the toll it often takes on patients’ quality of life (QoL). Most of the estimated 2.5 million Americans with at least moderate TR are of Medicare age, so a CMS coverage decision on these new therapies looms large for this population.
Diuretics can be used to manage symptoms in less severe cases of TR, but medical therapies have limited efficacy for the condition. Open surgery is an option for some patients with significant TR but has traditionally not been widely used. “The surgical community is increasingly aware of the benefit of early intervention, and the threshold to intervene on the tricuspid valve in conjunction with concomitant left-sided valve surgery has become lower,” notes Cleveland Clinic cardiothoracic surgeon Shinya Unai, MD. “However, the operative risk for isolated tricuspid valve surgery is high, mainly due to patients with long-standing severe TR developing liver and kidney dysfunction due to congestion. The need for other, less invasive options has long been recognized.”
Advertisement
Both the Evoque and TriClip transcatheter systems were deemed “breakthrough” devices by the FDA to help facilitate patient access. “At Cleveland Clinic, we’ve had the opportunity to treat patients with both devices over the past few years as part of their pivotal clinical trials,” notes Amar Krishnaswamy, MD, Section Head of Invasive and Interventional Cardiology. “With confirmation of the benefit of these devices based on the trials, as well as the improved quality of life we have seen directly among our treated patients, we are excited that FDA approval will allow us to help more patients benefit from these therapies.”
Despite this enthusiasm, which is shared by many other physicians who treat patients with TR, adoption of these devices is expected to be slowed by initial gaps in the evidence supporting their use, which stems from a somewhat lower evidentiary bar for approvals under the FDA’s breakthrough device designation.
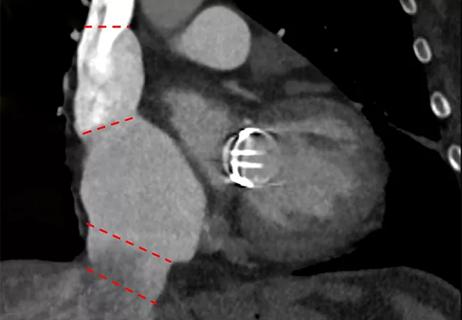
Approval of the Evoque system was based on a prespecified analysis of six-month results from the first 150 patients in the TRISCEND II pivotal trial, which has randomized 400 patients with severe or torrential TR to Evoque or optimal medical therapy. These early results, presented at TCT 2023 last October, revealed a lower-than-expected rate of major adverse events at 30 days (the primary safety endpoint). It also found that 98.8% of Evoque recipients achieved six-month reduction of TR grade to moderate or less and 93.8% to mild or less, and investigators reported “meaningful improvements in functional status and symptoms at six months” relative to medical therapy alone. One-year results from the full cohort — including all-cause mortality, tricuspid intervention and heart failure hospitalization — are expected at TCT 2024 in late October.
Advertisement
While the open-label TRILUMINATE trial that supported approval of the TriClip system has been published (N Engl J Med. 2023;388[20]:1833-1842), it showed significant improvement versus control (optimal medical therapy) only in terms of Kansas City Cardiomyopathy Questionnaire (KCCQ) score, a QoL measure, not in all-cause mortality or hospitalization for heart failure. A subsequent analysis of TRILUMINATE (J Am Coll Cardiol. 2024;83[1]:1-13) bolstered confidence in true treatment benefit by demonstrating that KCCQ score independently correlated with residual TR, but questions about the therapy’s effect on clinical events remain.
Studies of both transcatheter tricuspid valve procedures have been limited by the impracticality of using tricuspid valve surgery as a feasible control therapy at scale in a clinical trial setting. Dr. Kapadia notes that this distinguishes early clinical testing of these procedures from the early development of transcatheter aortic valve replacement (TAVR) and percutaneous mitral valve procedures, which both had viable surgical counterparts to serve as comparators. Moreover, sham-controlled studies face the challenge of maintaining blinding for 12 months or more and, in the case of transcatheter tricuspid valve replacement, ethical issues around giving anticoagulation to a placebo group.
Because the new tricuspid devices currently lack the depth of clinical trial evidence typical for most other device approvals, CMS is expected to require an extensive national coverage analysis to determine for which patients and under what circumstances reimbursement should be offered.
Advertisement
Questions to be grappled with include patient selection, imaging techniques required, and which procedural and clinical outcomes matter most. The question of patient-reported outcomes is particularly germane for patients with TR, as QoL considerations tend to be disproportionately important to this patient population, more so than for populations with most other heart valve diseases.
Insights on these questions will come from postapproval study requirements, which figured into the approvals of both devices, and from real-world data sources such as the TVT registry.
Meanwhile, the CMS national coverage analysis process will include hearings and public comment, during which at least half a dozen relevant medical/surgical societies are expected to weigh in. Dr. Kapadia expects that a national coverage determination from CMS could be finalized by the end of 2024.
He anticipates that any coverage decision will demand a careful clinical rollout of the new technologies, both because of the limited data and experience to date and because of the comprehensive, multidisciplinary management required for safe and optimal use of the devices.
“The heart team required for transcatheter tricuspid valve therapy is even a bit broader than what’s needed for aortic or mitral valve care,” Dr. Kapadia says, citing several specific reasons:
Advertisement
Additionally, a broad heart team approach ensures that surgery is considered for patients who are appropriate candidates, Dr. Unai points out. “Open surgical intervention is a good and effective option for many patients and can be done with acceptable risk in appropriately selected patients,” he says, citing a recent Cleveland Clinic study (J Thorac Cardiovasc Surg. 2023;166:740-751.e8).
According to Dr. Kapadia, in addition to the interventional cardiologist who may perform the transcatheter tricuspid procedure, the heart team for counseling and managing the care of these patients should include a cardiac surgeon, a heart failure cardiologist, an electrophysiologist and a cardiologist with specialty imaging expertise.
For this reason, he notes, CMS is expected to lay out guidance for which hospitals and operators can perform transcatheter tricuspid valve procedures. He expects the ultimate number of sites in the United States to be around 250 — much lower than the approximately 850 that now perform TAVR or the 500-some that perform transcatheter mitral valve procedures.
Dr. Kapadia believes that two good criteria for performing these new procedures are how many tricuspid valve surgeries a center currently does, to demonstrate that patients can be offered alternatives, and how many transcatheter mitral valve procedures a center performs. “Mitral valve procedures are more similar to the tricuspid procedures than TAVR is, so they are a better indicator of relevant experience,” he explains.
At the individual level, he believes that experience doing 25 transcatheter tricuspid valve procedures is a reasonable threshold for privileging physicians to perform them on their own.
It is uncertain whether and how a CMS national coverage determination will differ for the two transcatheter tricuspid devices approved to date, but clear differences between the therapies exist.
“There’s currently no understanding of whether one or the other device is better,” Dr. Krishnaswamy notes. “Our decision-making between the two will be based primarily on a thorough analysis of a patient’s anatomy and other patient-specific factors.”
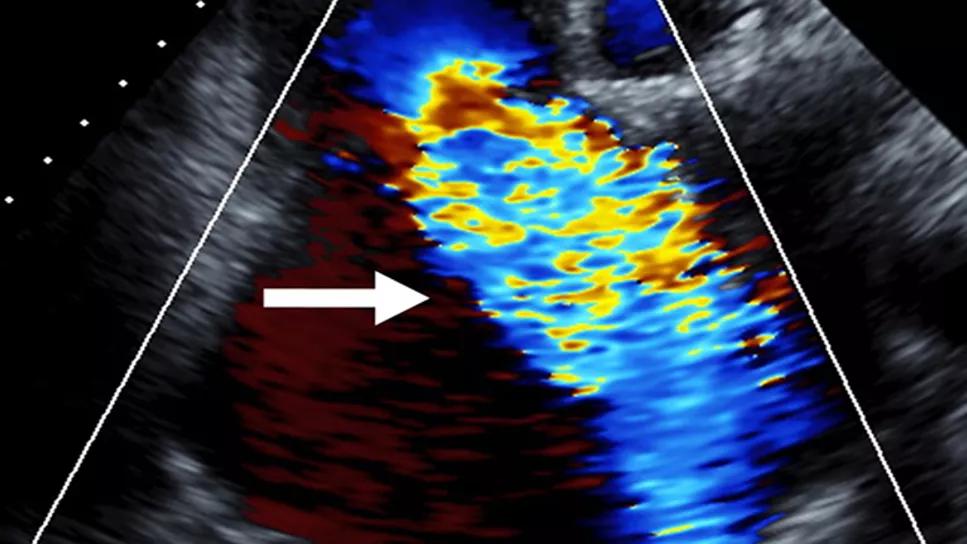
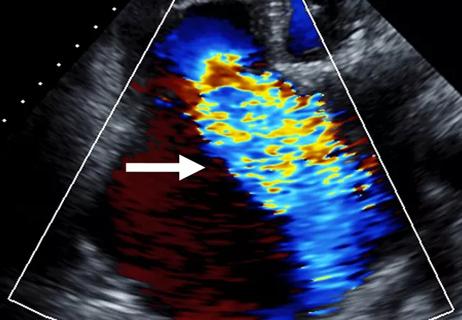
For instance, the TriClip’s TEER approach is not appropriate for patients with large coaptation gaps, a highly dilated annulus or pacemaker leads that prop the valve open too much. In contrast, valve replacement with the Evoque device will likely require anticoagulation therapy, appears to confer greater pacemaker risk and requires multiple exposures to contrast dye, which poses risk to patients with kidney dysfunction. And the durability of the replacement valve is unknown, although it’s likely to be similar to the seven to 10 years observed with surgical replacement valves, Dr. Kapadia says.
“If repair with the clip device seems highly feasible in a given patient, it may become the first choice,” he concludes, “whereas valve replacement will be the choice if the coaptation distance is too long.”
Advertisement

Study supports addressing mitral regurgitation before mild tricuspid regurgitation progresses

TRISCEND II trial reports 1-year results
Cleveland Clinic study argues against waiting for symptoms to develop
TEER is found to be a safe and good option for severe TR in select patients
Understanding VC anatomy is critical for transcatheter tricuspid valve interventions

A scannable graphic recap of our latest data

Aortic valve replacement is best option for lowering mortality in this high-risk population
Join us in New York Dec. 6-7 for broadened version of a CME crowd-pleaser