Cleveland Clinic study argues against waiting for symptoms to develop
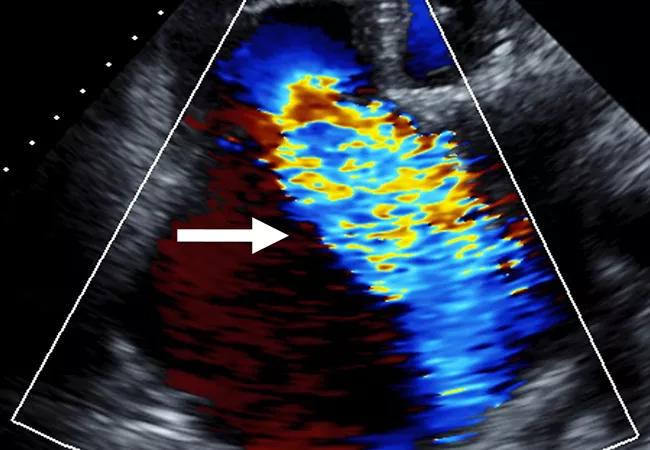
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/07fdbb80-5f65-4b0a-88b8-7769769cdc49/23-HVI-4078932_severe-tricuspid-regurgitation_650x450_jpg)
23-HVI-4078932_severe-tricuspid-regurgitation_650x450
Surgery should be considered for isolated severe tricuspid regurgitation (TR) before overt symptoms develop. So concludes a retrospective study of 159 patients who underwent isolated surgical tricuspid valve (TV) repair or replacement at Cleveland Clinic. The study was published in the Journal of Thoracic and Cardiovascular Surgery (2023;166[1]:91-100).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The investigation found higher operative mortality and significantly worse composite morbidities in patients who had symptomatic severe TR preoperatively compared with asymptomatic patients with severe TR and right ventricular dilation and/or dysfunction. The study is one of the largest single-center series of isolated TV surgery to date, and the first to compare surgeries by indication.
“We found that taking an earlier approach to intervening for isolated TR saves lives,” says senior and corresponding author Milind Desai, MD, MBA, a cardiologist and Director of Clinical Operations in Cleveland Clinic’s Department of Cardiovascular Medicine. “Waiting for symptoms to appear is associated with many comorbidities and higher patient risk for surgery.”
Isolated TV surgery entails higher risk of operative mortality than isolated operations on other heart valves or on coronary arteries. For this reason, it is not often performed even at high-volume centers like Cleveland Clinic, despite poor outcomes associated with severe TR.
The latest American College of Cardiology/American Heart Association guideline for valvular heart disease has no class I indications for isolated TV surgery, while European Society of Cardiology (ESC) guidelines have just one such indication — for severe symptomatic isolated TR.
The study population consisted of 159 patients who underwent isolated TV surgery at Cleveland Clinic between 2004 and 2018. Of those, 115 were symptomatic (“class I group,” per the ESC guidelines) and 44 were asymptomatic (“early surgery group”) at the time of surgery. At baseline, all patients in the early surgery group had one of the following: both right ventricular dilation and dysfunction (n = 12; 26.8%), right ventricular dilation alone (n = 23; 52.7%) or right ventricular dysfunction alone (n = 9; 20.5%).
Advertisement
Seventeen surgeons performed the procedures. Valve repair was performed in 73.0% of class I patients and 79.5% of early surgery patients (P = 0.54). More than 90% of valve replacements were done using bioprosthetic valves.
The two groups differed significantly at baseline in several respects: class I patients were older (mean age of 61.7 vs. 54.4 years; P = 0.016); had a higher prevalence of secondary TR (65.2% vs. 38.6%; P = 0.004); had more symptoms (by definition), including right heart failure, higher New York Heart Association class and greater likelihood to be in a critical preoperative state; and more often had a history of cardiac surgery, cardiac implantable electronic device, heart failure, atrial fibrillation or chronic lung disease than the early surgery patients.
Key findings were as follows:
The early surgery group had superior survival rates over the length of the study (mean follow-up, 5.1 ± 4.0 years). Multivariable analysis revealed that mortality during follow-up (the primary endpoint) was associated with the following factors:
Advertisement
“Although differences in outcomes between the two groups were mostly explained by baseline clinical differences, the early surgery group was still better off after adjustment for these differences,” Dr. Desai observes.
The study authors emphasize the following takeaways from their findings:
Advertisement
“Although this study has the limitations of a single-center observational investigation, it has the advantage of reflecting real-world practice,” Dr. Desai notes. “Randomized controlled trials are now needed to compare outcomes of surgical, transcatheter and medical management, along with their timing and indications.”
Advertisement
Advertisement
Study supports addressing mitral regurgitation before mild tricuspid regurgitation progresses
TRISCEND II trial reports 1-year results
Limited data and experience will translate to a cautious rollout
TEER is found to be a safe and good option for severe TR in select patients
Understanding VC anatomy is critical for transcatheter tricuspid valve interventions
A scannable graphic recap of our latest data
Aortic valve replacement is best option for lowering mortality in this high-risk population
Join us in New York Dec. 6-7 for broadened version of a CME crowd-pleaser