On the need for coordinated care
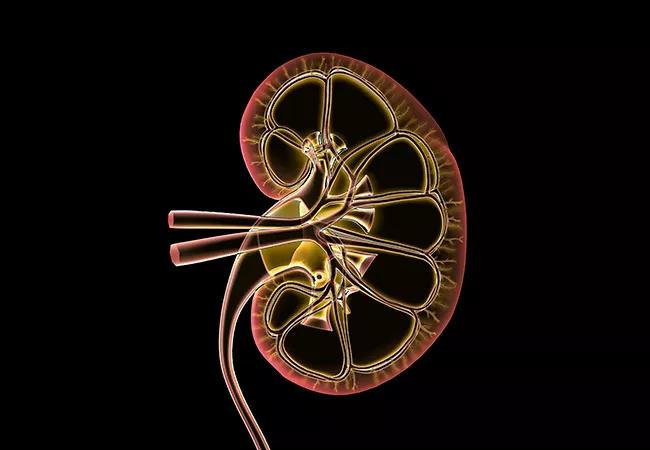
Children with chronic kidney disease (CKD) treated at Cleveland Clinic Children’s have a new champion in Amy Bobrowski, MD, who was recently appointed Head of Pediatric Nephrology and Medical Director of Pediatric Kidney Transplantation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Bobrowski honed her knowledge and skills at the Ann & Robert H. Lurie Children’s Hospital of Chicago, where she completed her fellowship in pediatric nephrology, followed by serving more than a decade on the faculty of the Division of Kidney Diseases and as Medical Director of Pediatric Kidney Transplantation. She was enticed to leave Chicago by the opportunity to grow the program at Cleveland Clinic Children’s.
“Children with kidney disease are best served in a system where all aspects of their care can be managed,” she says. “They need coordinated care with subspecialty and multidisciplinary support and good communication between specialists. We have that here at Cleveland Clinic Children’s,” she says.
“In addition, the available expertise in chronic kidney disease (CKD) and renal transplantation in adults is a huge benefit of being at Cleveland Clinic.”
Being diagnosed with chronic renal disease (CKD) at a young age puts patients at lifelong risk for serious medical problems that go beyond kidney function. These include:
These issues require coordination of care with other pediatric subspecialists and specialty support staff. Cleveland Clinic Children’s has a dedicated pediatric renal dietitian, who focuses on optimizing nutrition before and after transplantation. The team also includes a dedicated pediatric renal social worker, who works with pediatric psychologists, if needed, to address behavioral, psychiatric and cognitive issues.
Advertisement
“We modify whatever we can to help these patients live as long as possible with the best quality of life possible,” says Dr. Bobrowski.
Because the patients’ needs do not end after puberty, Dr. Bobrowski is part of a team developing a program for adolescent patients transitioning into adult care. She is in the process of identifying the adult providers who are interested in caring for these patients.
“We think it will be more effective to have a small number of providers who will eagerly accept these kids and be their champions,” she explains. “They must understand the unique challenges involved in caring for teens moving into adulthood and be invested in helping us create an environment for success during this challenging, higher risk period.”
Unlike most adult patients with CKD, the majority of pediatric patients suffer from congenital abnormalities of the kidney and urinary tract or hereditary diseases.
Transplantation does not provide a definitive cure, and chronic medications and close monitoring remain crucial for continued health. It does, however, have a definite advantage over staying on dialysis. “Both the survival and quality of life outcomes are far better after transplant than with dialysis,” says Dr. Bobrowski.
“Our goal is to minimize the time kids with CKD spend on dialysis or to eliminate it altogether when possible with pre-emptive transplantation [kidney transplantation performed before the need for dialysis is reached].”
The change in lifestyle from pre- to post-transplant is often a difficult transition for young patients to make. It requires patients to be closely monitored while families and older patients receive intensive education.
Advertisement
“We have to balance the risk of taking antirejection medications with the risk of infection,” says Dr. Bobrowski. “The medications have side effects. And since each child’s immune system is different, the post-transplant protocol must be personalized and remain flexible over time.”
Because CKD can present at any age, Dr. Bobrowski receives referrals from obstetricians, neonatal intensivists, urologists, pediatricians, pediatric cardiologists and family practitioners.
“We encourage physicians to involve us early, when we have the greatest chance of delaying disease progression or being best able to intervene to optimize growth and development,” she says.
She considers referring pediatricians important members of the patient’s care team.
“We depend on them to provide routine health maintenance, including vaccines. Children must have up-to-date vaccines to be listed for transplantation,” she says.
The diagnosis of CKD in a child is a frightening experience for families. With experienced, well-coordinated medical care, support and education, most now survive the diagnosis. The need persists, however, for structured multidisciplinary care and support for these patients and families, minimizing trauma and allowing them to move ahead with as normal of a life as possible.
“I love that we are able to see patients and families through what used to be almost universally fatal diseases,” says Dr. Bobrowski. “With the help of dialysis and transplantation, we are able to offer our patients a full and productive adulthood.
Advertisement
“Seeing these kids go through many challenges and start growing and living full and happy lives is very rewarding.”
Advertisement
Advertisement

Findings hold lessons for future pandemics

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes