The benefits of this emerging surgical technology
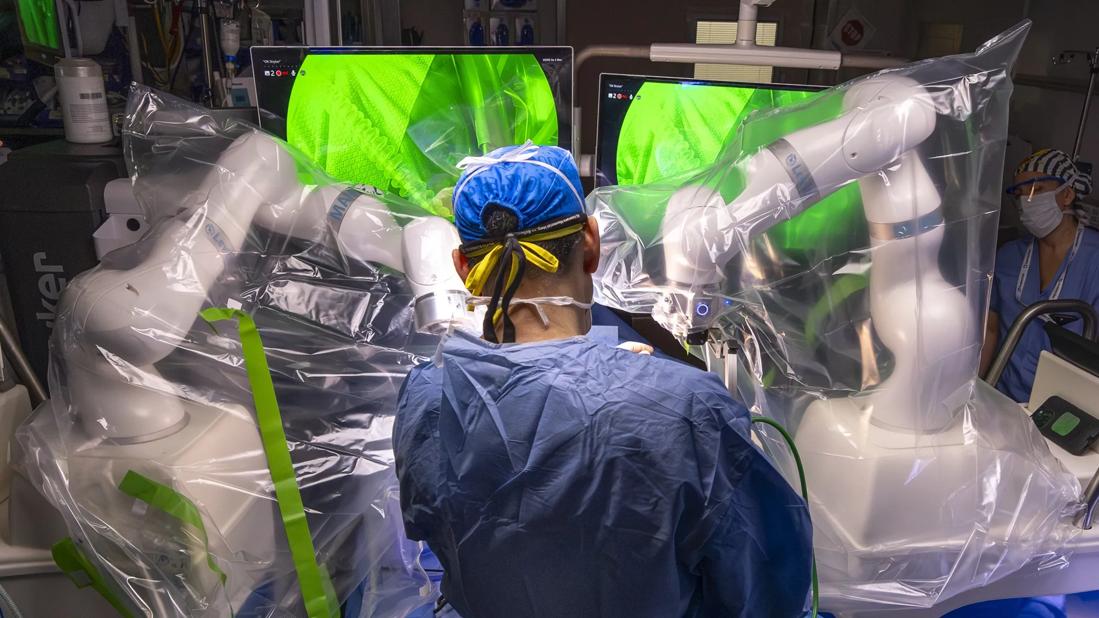
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/59ef3078-e8d9-4e4b-8e02-e758a02a59c3/childrens-gallbladder-magnetic)
Dr. Guelfand in the operating room
A Cleveland Clinic Children’s pediatric surgeon is the first to perform a laparoscopic cholecystectomy using magnetic-assisted surgical technology in a pediatric patient. The surgery follows a recent FDA clearance that expands the use of the surgical system to include patients age 12 and older. The result has enabled an even less invasive approach to laparoscopic cholecystectomy, paving the way for continued surgical innovation for young patients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In any patient population, but particularly in children, our goal is to minimize trauma and complications and improve pain, recovery and cosmesis,” says Miguel Guelfand, MD, Section Head General and Thoracic Surgery, Cleveland Clinic Children’s. Standard laparoscopic surgery for these patients typically requires four to five incisions, but the proprietary magnet-assisted technology makes the same surgery possible with only three incisions.
Though relatively rare in children, gallstones, also known as cholelithiasis, have been on the rise in recent decades. This increase is multifactorial, but many experts cite the quality of food and growing rates of obesity among children in the U.S. Cholecystectomy is almost always recommended for patients age 6 and older.
The patient, a 16-year-old female, presented to gastroenterology with severe abdominal pain, which was later confirmed by ultrasound to be caused by gallstones. The gastroenterology team referred her to Dr. Guelfand, who, after reviewing the imaging and speaking with the patient, affirmed that surgery was the best course. Two weeks later, the patient underwent the procedure.
Levita® Magnetics is the first company to offer magnetic technology for minimally invasive surgery—and is now the first to complete this type of surgery in a pediatric patient in the U.S.
Following a tiny incision, a special laparoscopic tool was inserted through a laparoscopic trocar through the patient’s abdomen, and a metallic clip was placed to grab the gallbladder. In this case, an external magnet was used to retract the gallbladder without any extra incision.
Advertisement
Magnetic surgery confers benefits to both the surgeon and the patient, according to Dr. Guelfand. The external magnet can hold or move organs inside the abdomen during surgery. Without it, an additional incision would have been required so that a surgical assistant could hold the gallbladder in place with a laparoscopic instrument. It also allowed for clearer visualization of the surgical field, he explains.
In addition to fewer incisions and fewer instruments inside the patient’s body, the system grants surgeons greater autonomy. “With the pedals of the surgical system, you’re controlling one robotic arm with the scope and the other with the magnet.
Dr. Guelfand says the surgery went “perfectly,” and the patient continues to recover well, as noted during a two-week postoperative visit; he will see her again at a two-month postoperative appointment. Dr. Guelfand anticipates she will return to a normal, pain-free life.
What pediatric surgeons should know— and a look ahead
Regarding the user experience, he offers the following to his peers: “This robot still gives you a traditional laparoscopic surgery experience but with the aid of a magnetic surrounding.” He calls it a “user-friendly, easy-to-access technology.”
With the expanded FDA clearance, patients ages 12 and older with the indicated conditions are now candidates for the magnetic-assisted technology, which includes pathologies beyond cholelithiasis. Dr. Guelfand has since completed another case and is planning more in early 2026. “It’s now part of our toolbox,” he adds.
Advertisement
“Cleveland Clinic Children’s is the first center in the U.S. to have and use this surgical system, and now we're going to continue exploring new avenues to improve the quality of care for our young patients. Less trauma and fewer incisions make sense to everyone,” concludes Dr. Guelfand.
Advertisement
Advertisement
Findings hold lessons for future pandemics
One pediatric urologist’s quest to improve the status quo
Overcoming barriers to implementing clinical trials
Interim results of RUBY study also indicate improved physical function and quality of life
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
Integrated care model reduces length of stay, improves outpatient pain management
A closer look at the impact on procedures and patient outcomes
Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve