Encouraging early outcomes in a challenging population
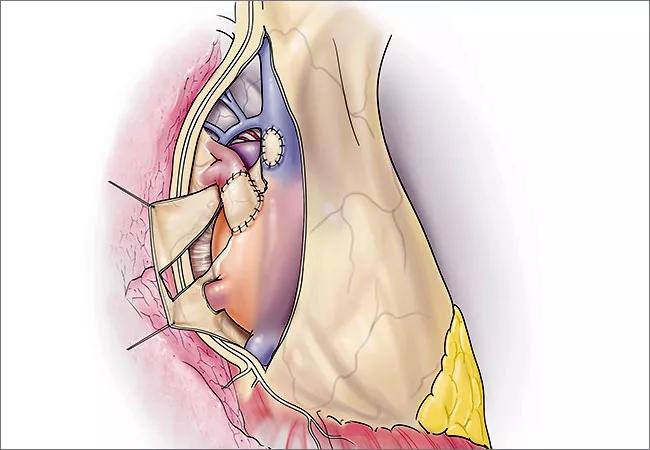
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0c6f914d-5b07-47c9-80c1-53903421f742/650x450-Distal-PA_pericardium-roll-up-4_19-HVI-1794810_jpg)
650×450-Distal-PA_pericardium-roll-up-4_19-HVI-1794810
By Tara Karamlou, MD, MSc, and Hani K Najm, MD, MSc, FACC
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Contemporary techniques for surgical repair of anomalous pulmonary veins (APVs) that are remote from the left atrium, either because of their remote insertion or because of associated complex cardiac anatomy, have shortfalls. Described repairs for this entity include mobilization and direct reimplantation into left atrial wall, use of interposition grafts, or creation of an intra-atrial baffle from the orifice of the anomalous veins to the left atrium through a pre-existing or constructed atrial septal defect (ASD).1,2,3 The Warden procedure, double-patch technique and the single patch-techniques are variations within the intra-atrial baffle genre, and are commonly utilized for treatment of remote right upper and sometimes right middle pulmonary veins. However, in all the aforementioned instances, there is a significant and unacceptable incidence of early and late pulmonary venous obstruction requiring percutaneous or surgical reintervention, as well as a risk of sinus node dysfunction. The risk of postoperative obstruction is increased with circular direct anastomoses, acute angulation of veins, or the need for increased mobilization and handling or clamping of the veins at the time of surgery. Scimitar veins, in which the anomalous right pulmonary vein has a very long vertical course (Figure 1), are especially prone to these complications.
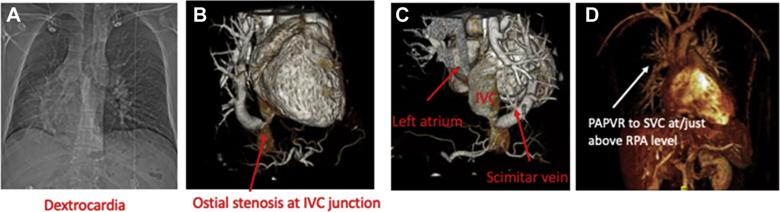
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7aede194-add0-45f9-81d1-1392ac869b3e/fig-1_jpg)
Preoperative evaluation with (A) chest radiograph, (B) computed tomography angiography, and (C) reconstructions demonstrating anatomy for 1 complex patient with scimitar syndrome and dextrocardia. (D) Common anatomy suitable for this technique: the right upper and middle pulmonary veins drains to the superior vena cavae (SVC) at or above the level of the right pulmonary artery (RPA). (IVC, inferior vena cava; PAPVR, partial anomalous pulmonary venous drainage.)*
Advertisement
The problems encountered with conventional repairs of APVs motivated the conceptualization of a novel method that uses an in-situ pericardial roll, similar to that initially described by Najm et al. in Scimitar syndrome.4 The basic tenet of this technique is that, through creation of a vascularized in-situ pericardial roll, the natural reflections of the pericardium can be leveraged to direct the anomalous venous return to the left atrium without complex baffles or need to manipulate the APVs themselves. We have completed this repair in six consecutive patients between 3 months to 65 years of age in the past year, with excellent early outcomes.5 The variability in age speaks directly to the versatility of this technique, which can be utilized in multiple morphologic arrangements. The different anatomic configurations and demographics of our early experience are shown in Table 1.
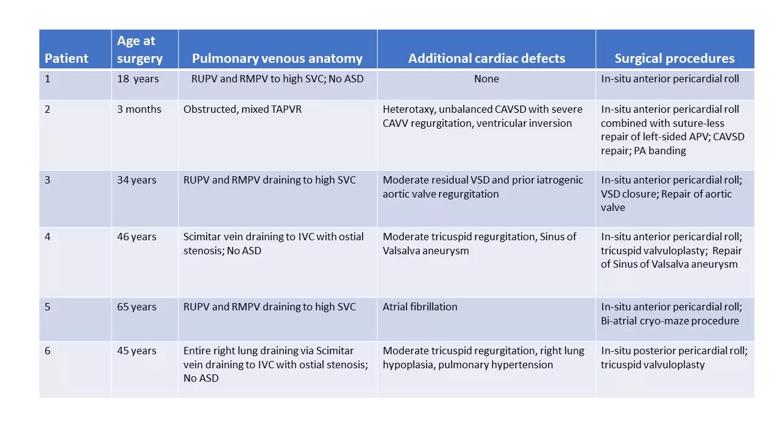
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e1c64487-99d1-4011-87d7-6077a6324ad6/STSA_APV_Table1_110519_jpg)
The major component steps of the operation for APV in which the pericardial roll lies anteriorly are delineated in Figure 2. For Scimitar syndrome, some modifications are needed, as shown in Figure 3. Some pearls of this technique include: 1) avoid encircling the inferior vena cava during the initial dissection in order to preserve the natural anatomic plane between the left atrium and the pericardial reflection; 2) the pericardium on the ipsilateral side to the APVs must be dissected widely; 3) the phrenic nerve should be completely mobilized using only sharp dissection; 4) femoral vein cannulation, rather than cannulation of the IVC directly, can improve visualization and facilitate use of the pericardial roll technique – especially in the anatomic case of Scimitar syndrome; 5) use of osteoplasties with medial opening of the Scimitar vein can be performed to relieve the native stenosis of the Scimitar vein with the IVC.
Advertisement
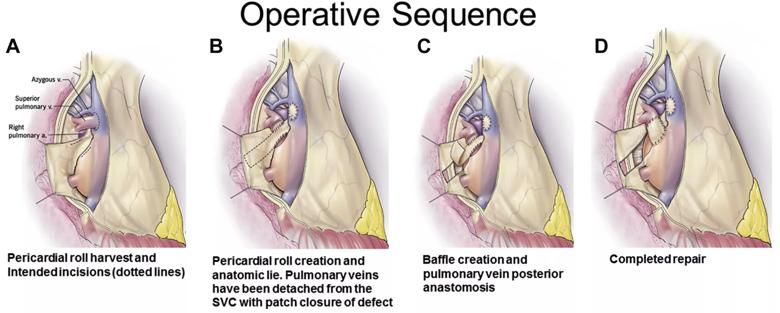
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/96c7adf3-94f8-4658-9a10-e5c3d42ccd27/fig-2-scaled_jpg)
Figure 2. (A-D) Surgical sequence as depicted by the artist for typical anterior pericardial roll technique for reconstruction of anomalous pulmonary veins distant from the left atrium. (SVC, superior vena cava.)*
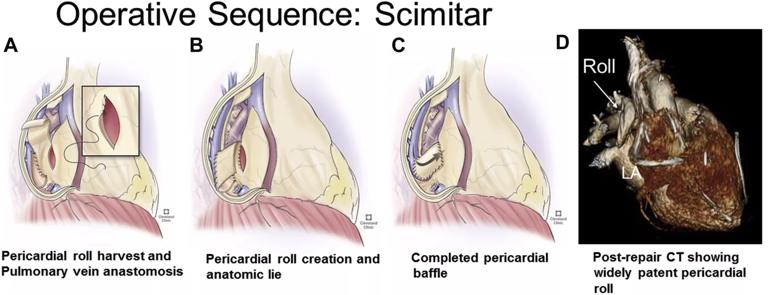
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f3a7a465-fdbc-4d1a-8057-15b9e9f926c0/fig-3-scaled_jpg)
Figure 3. (A-C) Surgical sequence as depicted by the artist for pericardial roll technique used in scimitar syndrome and (D) postoperative computed tomography (CT) reconstruction showing widely patent pericardial roll repair.*
There have been no mortalities. Median hospital stay was 23 (range 4-60) days. Median follow-up time is 20 (1 -36) months. Two patients underwent reinterventions to address narrowing of one of the right upper pulmonary veins. The first was an infant with single ventricle, heterotaxy and mixed total anomalous pulmonary venous return (TAPVR), in whom the in-situ pericardial roll technique was used as one component of a complete repair of TAPVR. Following repair, the infant required percutaneous dilatation of the right upper pulmonary vein and stenting of left atrial anastomosis. He has subsequently undergone complex ventricular switch, as described by our group,6 to convert him from a single ventricle circulation to a 1.5 ventricle circulation. Importantly, following TAPVR repair using this combined approach, his pulmonary hypertension has resolved completely. The other patient, an adult who had multiple prior percutaneous interventions (including multiple pulmonary vein isolation procedures) to address atrial arrhythmias, required reoperation to revise the pericardial baffle on postoperative day two, and subsequent dilation and stenting of the right upper pulmonary vein five months later. At last follow-up, multi-modality imaging showed widely patent pulmonary veins to the left atrium (Figure 4). All adult patients are asymptomatic with excellent functional status (NYHA Class 1).
Advertisement
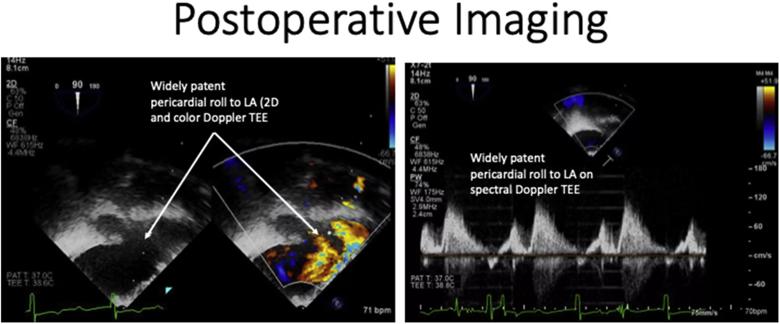
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f4af503e-2c4e-4975-a1cf-2eed1d6fb48d/fig-4-scaled_jpg)
Figure 4. Transesophageal imaging obtained immediately after surgery demonstrates a widely patent pericardial roll and non-obstructed flow pattern on spectral Doppler transesophageal echocardiography (TEE).*
This formative experience details extended use of the in-situ pericardial roll technique, using both superior and inferior configuration, to repair APVs that are distant from the left atrium, and characterizes the successful early outcomes in this challenging population. Our approach to this technique has been iterative in that we have made modifications based on intraoperative findings and subsequent postoperative course in several patients – a testament to the commitment of our expert multidisciplinary team.
The technique we describe is highly versatile, in that it can be utilized in multiple anatomic configurations and can be coupled with other techniques, such as contralateral sutureless repair, to address abnormal pulmonary venous drainage. Given that direct circumferential anastomosis of the delicate pulmonary veins is avoided, this technique is ideal for infants and in adults with multiple small, separate APVs. The early outcomes of the first six patients reported in this series are encouraging. Despite the two patients who required additional procedures, all patients have had excellent relief of their presenting symptoms and reassuring early imaging without diaphragm paralysis or phrenic nerve palsy.
Advertisement
*Note: Images used with permission; previously published in: Najm HK, Ahmad M, Salam Y, et al. Early outcomes for in situ pericardial roll repair for distant anomalous pulmonary venous return. Ann Thorac Surg. 2020 Apr;S0003-4975(20)30596-8.
Dr. Karamlou is a pediatric and congenital heart surgeon at Cleveland Clinic. Dr. Najm is Director of Pediatric and Congenital Heart Surgery at Cleveland Clinic.
Advertisement
After four decades, refinements to the gold standard of bypass continue as new insights emerge
Why definitive surgical closure is the gold standard, and new ways to make it possible
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon