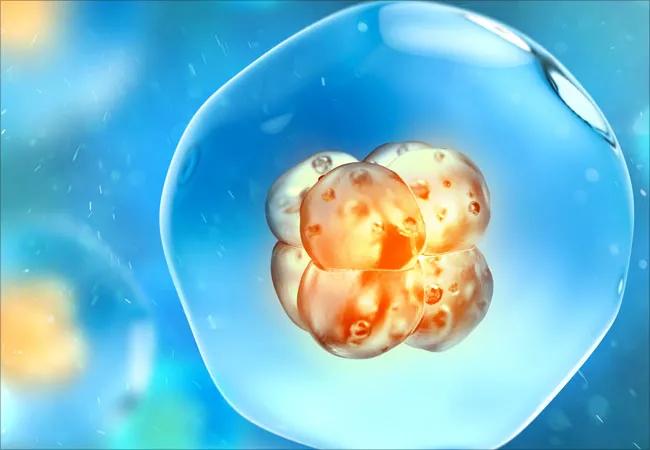
Study reveals another ranking criterion that may aid in embryo selection
A team of researchers using computer vision analysis of time-lapse videos of embryos ascertained that blastocyst pumping events have a high negative predictive value for subsequent failed implantation. Results of the study, led by Israeli-based AiVF, were presented at the American Society for Reproductive Medicine’s 2021 Scientific Congress & Expo.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The purpose of the study was to use artificial intelligence (AI) to deselect embryos that are less likely to implant,” says Nina Desai, PhD, HCLD, Director of Cleveland Clinic’s In Vitro Fertilization Lab and study co-author. “When we have five or six blastocysts, we use different criteria to rank them and give patients the best opportunity to get pregnant on their first or second transfer.”
Cleveland Clinic’s IVF Lab, which performs 100% blastocyst stage transfers, is one of a few clinics in the country that performs time lapse (TL) cultures of all patient embryos. The lab has five EmbryoScope® TL chambers that provide continuous imaging data on embryos, their morphology and their cell division kinetics from days 1 through 6 of development.
During development, the blastocyst pushes against the surrounding zona pellucida to expand. “Some embryos do this beautifully, while others struggle and go through a series of contractions and expansions, which you can see using time lapse videos,” says Dr. Desai.
Using AiVF’s AI-based digital embryology management platform, the researchers studied these contractions and expansions to see if blastocoelic contractions greater than 8 microns in diameter were associated with poor implantation rates independent of other morphokinetic features.
The team analyzed 148,441 images from time-lapse sequences of 317 expanded blastocysts chosen for transfer with known implantation data. It used the following definitions:
Advertisement
Researchers measured the number and extent of pumping events, as well as the stage of blastulation at which they occurred, and compared them to the known implantation outcomes of the embryos.
“We found differences in the number of weak contractions between embryos that implanted and those that did not implant,” says Dr. Desai. “We also found significant differences in major pumping events of more than 16 microns. The odds ratio was 1.8-fold higher for not implanting if the blastocyst showed a major pumping event.”
Of the 317 blastocysts studied, 188 (59.3%) successfully implanted. Among those, early pumping was noted in 27 (14%) blastocysts, while early pumping occurred in 22 (17%) of the 129 blastocysts that failed to implant. Major pumping events occurred in 14 (7%) blastocysts that implanted compared to 18 (14%) blastocysts that failed to implant. In addition, major pumping events were significantly correlated with implantation failure (OR 1.87, P=0.03 for at least one major pumping event and OR 2.42, P=0.04 for at least two major pumping events.)
Dr. Desai says the results of this study indicate that blastocyst pumping events can be used as one criterion to rank and deselect certain embryos, and AI tools make it possible.
“The next step in the world of IVF is to harness the power of AI to identify the embryo you want to transfer because of subtle features that give you a clue as to what’s happening inside of it,” she says. Ultimately, this benefits patients at Cleveland Clinic’s IVF Lab, which performs single blastocyst transfers, and IVF labs worldwide.
Advertisement
“IVF is very expensive, and we want patients to get pregnant in the first two cycles,” says Dr. Desai. “Being able to eliminate embryos that are less likely to implant shortens the time to pregnancy.”
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment