Study finds that in the absence of ACS, the yield is low and outcomes are unaffected
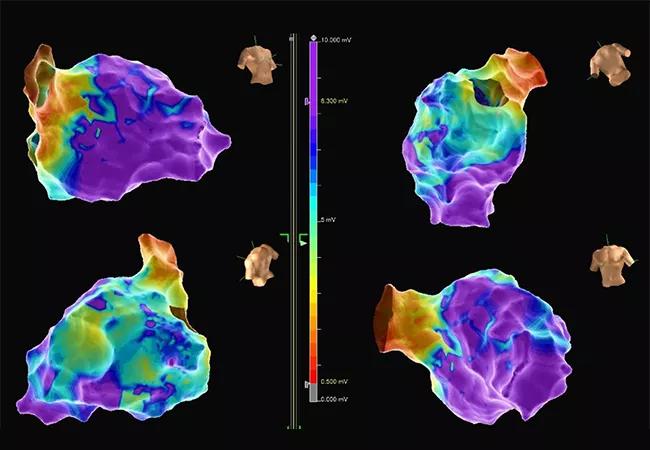
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4c06d22e-477d-484c-a7b9-76c6ee3adbd7/23-HVI-4194574-CQD-650x450-1_jpg)
maps for ventricular tachycardia ablation
Ischemic or coronary evaluations often unnecessarily delay lifesaving ablation therapy in patients who have monomorphic ventricular tachycardia (VT) electrical storm with no indication of an acute coronary syndrome (ACS). So concludes a retrospective study of nearly 100 patients from a Cleveland Clinic registry, which found that such evaluations resulted in low yield of findings of causative coronary occlusions and had little impact on procedural and mortality outcomes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study ― believed to be the first to address this issue ― was recently published in JACC Clinical Electrophysiology (2023;9[9]:1890-1899).
“In the setting of monomorphic VT electrical storm without ACS, we concluded that time and resources are generally better spent focused on prompt rhythm control than on coronary assessment,” says the study’s corresponding author, Ayman Hussein, MD, of Cleveland Clinic’s Section of Cardiac Electrophysiology and Pacing. “Ischemia assessment not only delays therapy but involves risks inherent to invasive coronary angiography.”
Monomorphic VT is increasingly prevalent as survival from various cardiomyopathies improves, leaving patients with scarred myocardium, which is thought to trigger the arrhythmia. The clusters of VT defined as electrical storm constitute a medical emergency and are associated with a high risk of death. Catheter ablation, which can reduce arrhythmia and improve outcomes, has become the primary management strategy.
Most experts agree that cardiac arrest from ventricular fibrillation or polymorphic VT merits exploration for a coronary or ischemic cause. But whether such evaluation is useful for patients with monomorphic VT-related electrical storm without indications of myocardial ischemia is unclear. However, such evaluations are commonly performed before ablation, and guidelines are silent on the issue.
The study population was drawn from a prospectively maintained Cleveland Clinic VT ablation registry. From 2014 to 2020, 97 patients with monomorphic VT storm without ACS (defined as angina or electrocardiographic indicators of ischemia) were identified (mean age, 64.2 years; 88.1% male).
Advertisement
Overall, the cohort had severe left ventricular dysfunction (mean left ventricular ejection fraction of 30.3%) and a median NYHA functional class of II. Notably, 67% had known ischemic cardiomyopathy, 35% had undergone previous coronary artery bypass grafting and 72% were known to have previous coronary disease. One-third of patients were in acute decompensated heart failure at the time of VT storm.
Of the 97 patients, 44 (45%) underwent ischemic or coronary evaluation before ablation, consisting of noninvasive myocardial perfusion testing (n = 25), coronary angiography (n = 10) or both (n = 9). No acute coronary occlusions were identified.
Four patients (4%) underwent coronary revascularization after evaluation, none of which was performed for acute coronary occlusion. All were successful procedures, but in all cases, VT reoccurred and ablation was required.
Mortality over mean follow-up of two years was 33% in those who had ischemic or coronary evaluation and 37% in those who did not (P = 0.646). Factors associated with mortality in unadjusted analysis were older age, worse left ventricular systolic function, higher number of antiarrhythmias before ablation and longer clinical VT cycle length. In adjusted analysis, only older age was associated with mortality.
“Features associated with death were similar to those associated with poor outcomes in heart failure,” Dr. Hussein observes. “Importantly, we found no link between ischemic evaluation and acute ablation outcomes or mortality during follow-up.”
Advertisement
A secondary analysis was performed among patients with monomorphic VT storm without ACS but with known coronary artery disease and regardless of ablation status. This was designed to help eliminate possible bias, as the primary cohort did not include potential patients with VT storm who underwent coronary assessment, were successfully revascularized and were not referred for ablation. Among the 91 patients in this secondary cohort, 46 underwent ischemic or coronary evaluation and 45 did not. Comparative results were similar to those of the primary analysis.
“Overall, coronary assessment didn’t change management, ablation strategy or outcomes,” Dr. Hussein notes. “Even when revascularization interventions were undertaken, they didn’t alter the course of the VT and the patients still needed ablation.”
“This study confirms that monomorphic VT in patients with structural heart disease typically indicates the presence of a scar-related reentrant circuit, with active ischemia playing a minimal role in its pathogenesis,” explains study co-author Pasquale Santangeli, MD, PhD, Medical Director of Cleveland Clinic’s Ventricular Arrhythmia Center. “It is unlikely that ischemic or coronary evaluation and/or revascularization will have a meaningful impact on VT recurrence, and most patients will ultimately require catheter ablation to obtain VT control.”
He adds, however, that since catheter ablation of VT is a complex and lengthy procedure, preprocedural ischemic evaluation may still be beneficial in some patients because it influences the VT ablation procedural approach in terms of number of VT inductions, use of isoproterenol to facilitate VT induction, and ablation strategy — e.g., targeting substrate in sinus rhythm versus attempting mapping and ablation during ongoing VT.
Advertisement
“More work will need to be done to identify the subset of patients who will never need ischemic workup before VT ablation,” notes study co-author Oussama Wazni, MD, MBA, Section Head of Cardiac Electrophysiology and Pacing at Cleveland Clinic.
In the meantime, consultation with an electrophysiologist is key to optimal patient management in this setting. “It is not uncommon to have patients with VT storm undergo an ischemia evaluation before an electrophysiologist is consulted,” Dr. Hussein observes. “We would urge our cardiovascular colleagues to involve us earlier so that we can help determine if further assessment is needed or if the patient can promptly undergo ablation.”
Advertisement
Advertisement
Procedure allows for safer epicardial VT mapping and ablation
Further study needed to assess potential role in select subgroups
New technology aids a Cleveland Clinic London patient with a complex arrhythmia
Multimodal evaluations reveal more anatomic details to inform treatment
A closer look at the impact on procedures and patient outcomes
Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve
Join us in Florida this winter for a long-standing CME favorite
Two cardiac surgeons explain Cleveland Clinic’s philosophy of maximizing arterial graft use