Procedure allows for safer epicardial VT mapping and ablation
Pericardial access for epicardial mapping and ablation for ventricular tachycardia (VT) is sometimes necessary to target areas that cannot be accessed from the endocardium. The standard procedure involving subxiphoid entry to gain access, first described by Sosa and colleagues in 1996, continues to be challenging. Because the pericardial cavity is normally a virtual space, risks of inadvertent right ventricle puncture and coronary artery injury remain substantial, limiting the procedure to highly experienced operators at specialized centers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Being able to access the epicardium has changed the way we do electrophysiology,” says Pasquale Santangeli, MD, PhD, Medical Director of Cleveland Clinic’s Ventricular Arrhythmia Center. “But it’s a procedure in need of innovation to make it safer and more accessible to operators in nonspecialty centers.”
CO2 insufflation of the pericardial cavity via intentional coronary venous perforation from the coronary sinus is emerging as an important method to create safer conditions, as it creates a large and visible target space for subxiphoid puncture. Dr. Santangeli was the first to bring the procedure to the U.S. and is currently one of a small number of users of the technique in the nation. He recently co-authored a step-by-step description of how it is performed in the Journal of Interventional Cardiac Electrophysiology (2023;66:109-116), and he reported on the method at Cleveland Clinic’s Global EP Summit 2023 in September. Key points of his talk are summarized below.
Since pericardial access techniques were introduced nearly 30 years ago, the current standard approach ― accessing the virtual space of the pericardial cavity via a subxiphoid approach with a Tuohy or micropuncture needle ― has not changed substantially. The technique is associated with a rate of complications up to 10%, highlighting the need for a safer strategy.
During this time, indications for epicardial access have expanded dramatically. Access to the pericardium is also needed to treat some cases of supraventricular arrhythmias and Brugada syndrome, as well as for left atrial appendage ligation with percutaneous epicardial devices. It could also be useful for annuloplasty and to obtain percutaneous access to the pericardium in patients with preexisting adhesions or localized effusions.
Advertisement
Dr. Santangeli led a review of 60 manuscripts from 1996 to 2013 for complications associated with standard percutaneous epicardial access. Out of 1,591 cases in which the procedure was done for VT, 97% achieved successful access. Major complications ― including hemopericardium, tamponade, right ventricle perforation and coronary artery damage ― occurred in about 4% of cases, with another 4% involving minor complications.
Dr. Santangeli outlined the major steps involved in CO2 insufflation of the pericardial cavity via coronary sinus distal vein perforation. He noted that under most circumstances, perforation of the coronary sinus does not result in significant bleeding because of the low systolic and diastolic pressure within the distal coronary sinus.
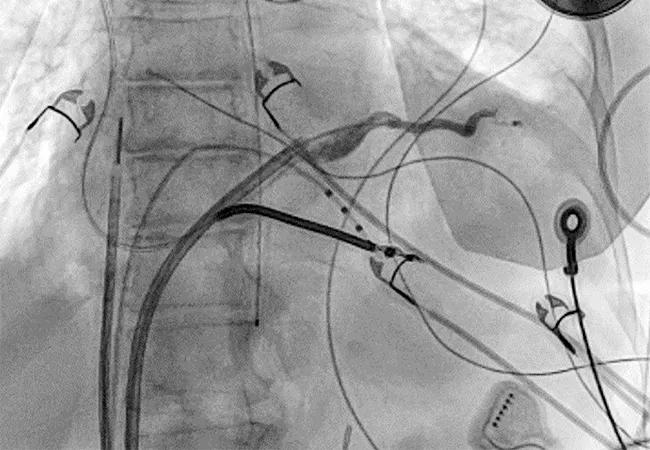
First, a coronary sinus venogram is used to select the target vessel for puncture (Figure 1). Via femoral venous access, an intracardiac echocardiography catheter (to evaluate pericardial effusion after coronary vein exit) and a deflectable sheath are advanced into the mid-right atrium. Any coronary vein with favorable anatomy and which allows apical cannulation can serve as the target vessel. About 90% of the time, a posterolateral branch of the coronary sinus is chosen.
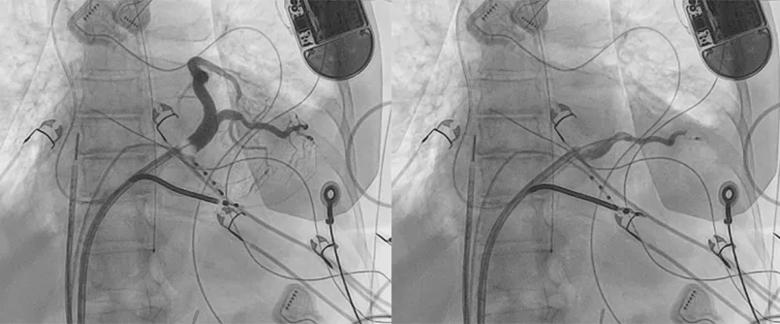
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/29f072eb-e21e-478d-bbb9-9bb6260400bc/23-HVI-4298713-CQD-Inset-1c_gif)
Figure 1. Videos depicting selection of the target distal coronary sinus branch for intentional perforation. (Reprinted, with permission, from Cerantola and Santangeli, J Intervent Card Electrophysiol.2022;66:109-116.)
After cannulation of the target vessel, exit is performed with a high-tip-weight coronary wire designed for chronic total occlusion interventions. Briskly advancing the wire to exit the coronary vein provides access to the pericardial cavity.
Advertisement
“After perforation of the coronary sinus, if the catheter bends and cannot be advanced into the pericardial space, it may indicate the presence of adhesions,” Dr. Santangeli warns (Figure 2). “At that point, we cross over to surgical epicardial access.”
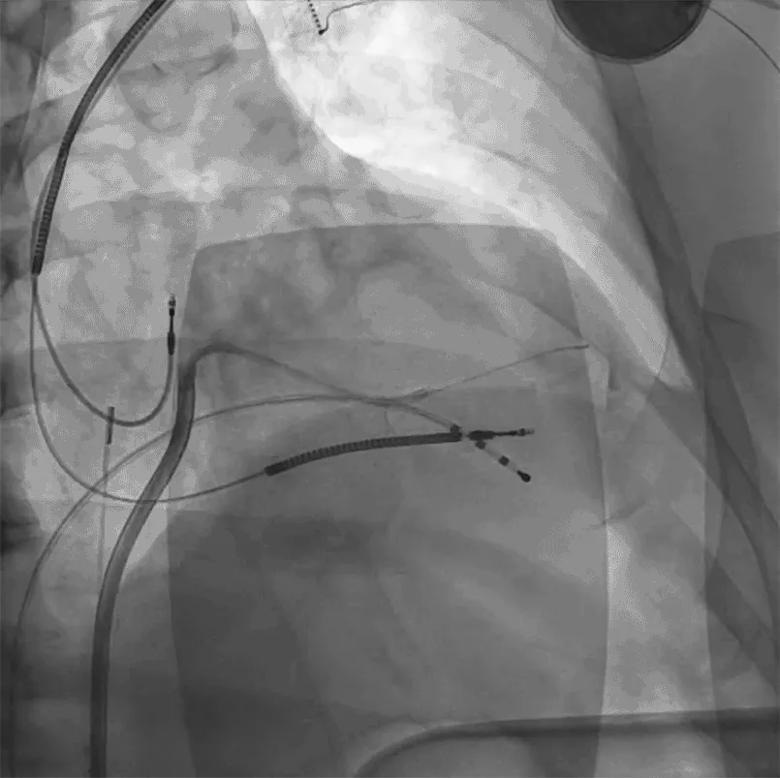
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d7e2692e-f071-4059-a431-e8370ba19284/23-HVI-4298713-CQD-Inset-2c_gif)
Figure 2. Example of pericardial adhesions in the posterolateral left ventricle in a patient with a history of prior epicardial ablation complicated by post-procedure pericarditis. (Reprinted, with permission, from Cerantola and Santangeli, J Intervent Card Electrophysiol.2022;66:109-116.)
After successful access, a CO2 contrast tank is connected to a syringe, and CO2 is slowly allowed to passively flow into the pericardial space until adequate separation is achieved (typically with 100-200 mL of CO2). A slight drop in blood pressure usually results but rarely requires intervention.
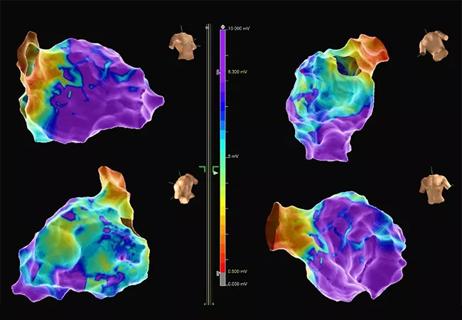
Because CO2 has a low molecular weight, it distributes anteriorly if the patient is supine, displacing pericardial fluid posteriorly (Figure 3). This is the opposite of injecting a contrast agent, which is heavier than pericardial fluid and therefore collects posteriorly.
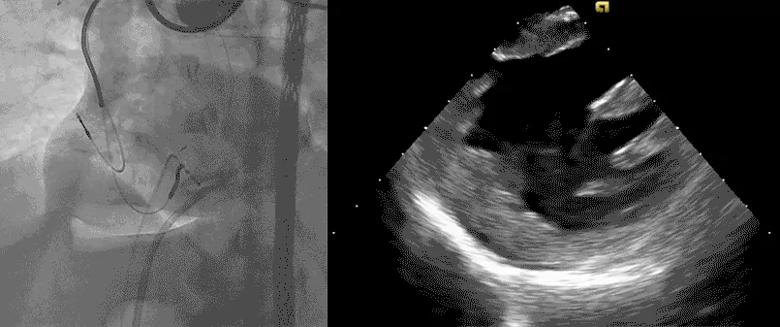
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/48167b86-9288-4cb7-8b24-d15d63422ec3/23-HVI-4298713-CQD-Inset-3c_gif)
Figure 3. Videos showing typical findings ― a drop in blood pressure but no posterior effusion, due to the fact that CO2 is lighter than pericardial fluid and is localized to the anterior right ventricle.
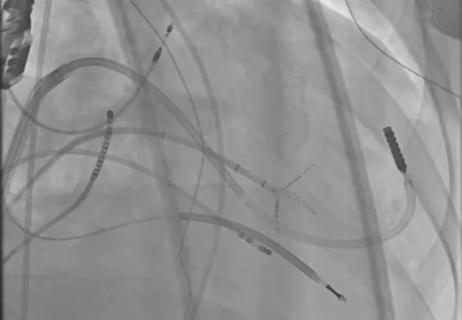
Once separation of the pericardial space is achieved, subxiphoid epicardial access can be conducted targeting the area of largest pericardial separation as seen by fluoroscopy (Figure 4). A needle preloaded with a wire is used to prevent pericardial deflation after access.
Advertisement
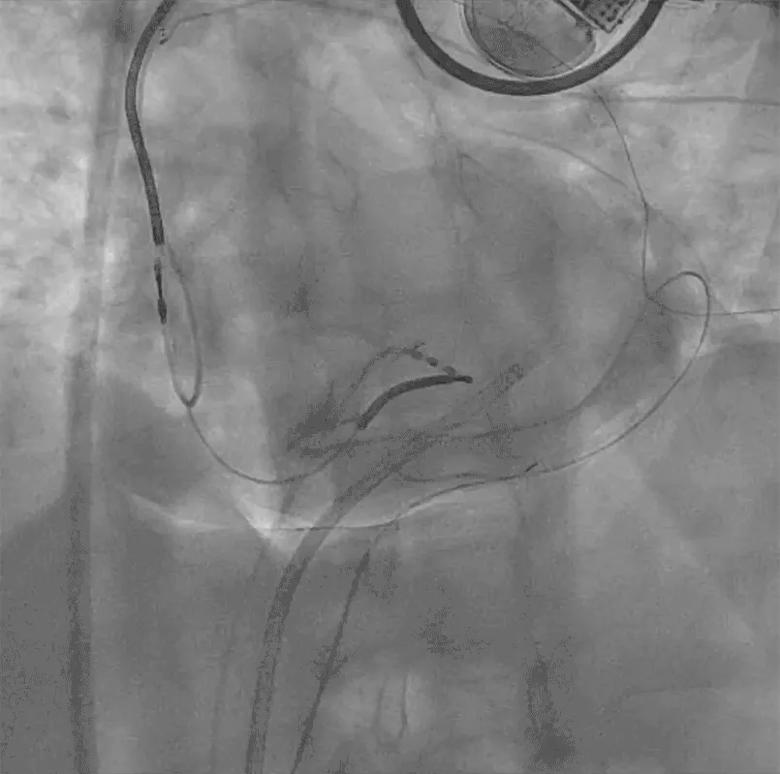
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7c42d904-f43d-4bd7-ba68-9338ba9a26df/23-HVI-4298713-CQD-Inset-4c_gif)
Figure 4. Video showing epicardial access targeting the area of largest pericardial separation on fluoroscopy.
Dr. Santangeli notes that the safety of coronary vein puncture in patients with advanced right ventricular failure and high right atrial pressures has yet to be established, and it is important to ascertain whether there is an excessive risk of bleeding in this situation.
In addition, safety for patients on uninterrupted oral anticoagulation is also unknown. “I suspect it’s safe,” Dr. Santangeli says. “But in most cases, oral anticoagulation is stopped, so it’s unlikely that this issue will ever be adequately studied.”
He adds that epicardial access using CO2 insufflation requires many steps, which can cause operators to become frustrated and switch to a conventional approach.
“We need better tools to minimize the number of required procedural steps,” he concludes. “Once we simplify the procedure and gain more experience, access to this procedure can be expanded to more operators.”
Ultimately, he adds, a prospective randomized trial comparing CO2 insufflation with “dry” entry into the pericardial space should be conducted.
“Given the substantial risks, pericardial access for epicardial mapping and ablation is currently performed only by centers with deep experience in VT ablation,” notes Oussama Wazni, MD, MBA, Section Head of Cardiac Electrophysiology and Pacing at Cleveland Clinic. “With the emergence of intentional perforation of cardiac structures with insufflation of CO2 to facilitate pericardial access, there is now a path forward to potentially expand this practice to more centers so that more patients can benefit.”
Advertisement
Advertisement
Study finds that in the absence of ACS, the yield is low and outcomes are unaffected

Further study needed to assess potential role in select subgroups
New technology aids a Cleveland Clinic London patient with a complex arrhythmia

Multimodal evaluations reveal more anatomic details to inform treatment

A closer look at the impact on procedures and patient outcomes

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve

Medical and surgical perspectives on current and emerging uses of ECMO and Impella

New review distills insights and best practices from a high-volume center