Retrospective analysis suggests so, and offers support for surgical valve fracture/modification too
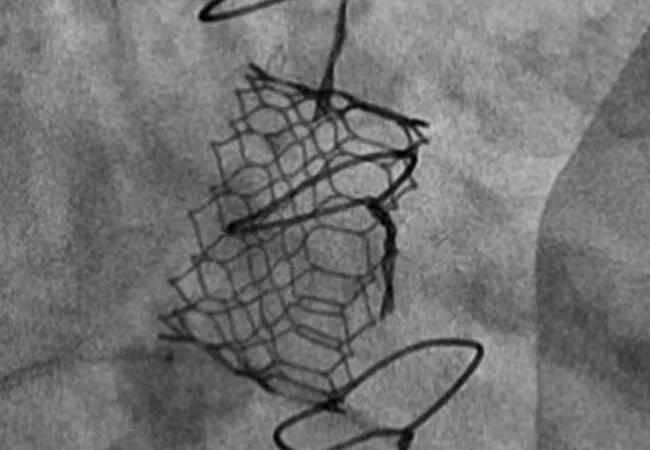
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/65335585-7f51-4b97-9260-221815cacb36/22-HVI-3073819_valve-in-valve-TMVR_650x450_jpg)
22-HVI-3073819_valve-in-valve-TMVR_650x450
The “minimalist approach” to anesthesia and imaging guidance used in many transcatheter aortic valve replacement (TAVR) cases appears to be feasible and safe for use in valve-in-valve (ViV) transcatheter mitral valve replacement (TMVR) as well. So concludes a research letter from a Cleveland Clinic team published in JACC: Cardiovascular Interventions (2022;15[12]:1288-1290).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Most operators currently perform valve-in-valve transcatheter mitral valve replacement with patients under general anesthesia using transesophageal echocardiography (TEE) for guidance,” says corresponding author Amar Krishnaswamy, MD, Section Head of Invasive and Interventional Cardiology at Cleveland Clinic. “We believe a minimalist approach to anesthesia can be applied in this procedure, and we have begun doing so in almost all patients for a few years now. We reviewed our experience to date to assess the effects of this strategy on patient outcomes.”
The minimalist approach involves use of either conscious sedation or monitored anesthesia care (MAC) in lieu of general anesthesia, with intracardiac echocardiography used in lieu of TEE. “This offers the advantages of minimized anesthetic requirements with expected reductions in patient recovery time and potential risks associated with endotracheal intubation and general anesthesia,” Dr. Krishnaswamy explains.
The researchers identified all patients (N = 56; mean age, 75 years) who underwent transfemoral-approach ViV TMVR at Cleveland Clinic from January 2012 through December 2020. Initial cases were all performed using general anesthesia, but after the group’s first three years of experience (2012-2014), operators could elect to perform the procedure with patients under either conscious sedation or MAC. Across all cases, transseptal puncture was guided either by intracardiac echo for patients receiving MAC/conscious sedation or by TEE for patients receiving general anesthesia.
Advertisement
Of the study’s 56 patients, 14 received general anesthesia and 42 received MAC or conscious sedation. There were no significant baseline differences between the two groups. Valve placement was successful in all cases, with no instances of paravalvular regurgitation and no mortalities at 30 days. Other 30-day clinical outcomes and longer-term outcomes were statistically comparable between the two groups, with one exception: mean hospital length of stay (LOS) was 50% shorter in the MAC/conscious sedation group (3 ± 3.4 days) than in the general anesthesia group (6 ± 6.2 days).
The researchers note that LOS declined steadily throughout the study period and was likely due in part to implementation of protocols to avoid postprocedure ICU care and facilitate earlier ambulation, “but the lack of general anesthesia/endotracheal tube is likely also a factor,” they write.
The reduced LOS associated with the minimalist approach offers at least two key benefits: reduced use of healthcare resources and a potential reduced risk of postprocedural delirium. “Elderly patients and those with comorbidities are at elevated risk of delirium in the hospital following a percutaneous valve procedure,” Dr. Krishnaswamy says. “It’s likely that this risk is reduced by minimizing anesthesia exposure, promoting earlier mobilization and returning the patient to familiar surroundings more quickly, although further study is needed to confirm this.”
He adds that choice of anesthesia approach should ultimately be guided by specific patient circumstances. “At Cleveland Clinic, we routinely use this minimalist approach for patients receiving valve-in-ring replacement, in view of the radiopaque landing zone,” he says, “but we use general anesthesia and TEE guidance for valve-in-valve replacement in the setting of mitral annular calcification, given challenges related to the fluoroscopic limitations of valve positioning.”
Advertisement
In addition to its anesthesia-related findings, the analysis yielded insights on a secondary research question: the impact of surgical valve fracture or modification for optimizing hemodynamics in ViV TMVR.
“Most surgical valves placed in the mitral position have a relatively rigid ring,” says Cleveland Clinic cardiothoracic surgeon Daniel Burns, MD, MPhil, a co-author of the research letter. “As a result, mitral valve-in-valve implantation can be limited by suboptimal valve expansion and hemodynamics, especially in patients who have received relatively smaller-size surgical valves.”
In response, Cleveland Clinic operators have begun to apply a method used to optimize hemodynamics in ViV TAVR — namely, high-pressure postdilation/surgical valve fracture — to ViV TMVR as well. Among the 45 cases from the current series undertaken after introduction of this adjunctive technique, 32 underwent high-pressure postdilation/surgical valve fracture, with surgical frames not undergoing fracture in just 11 cases. The decision not to fracture was driven by operator concern about limited space around the left ventricular outflow tract.
“In addition to demonstrating the feasibility and advantages of our minimalist approach to anesthesia, this analysis illustrates the feasibility of high-pressure postdilation for optimizing ViV hemodynamics in transcatheter mitral valve replacement, just as it is used in TAVR,” Dr. Burns notes.
“We are seeing more and more patients for mitral valve-in-valve procedures each year,” Dr. Krishnaswamy observes. “In fact, in the past year we have performed almost two-thirds as many of these procedures as were included in this entire study, which ran through the end of 2020. This demonstrates the increasing relevance of the minimalist approach.”
Advertisement
Advertisement
A new CME opportunity in Chicago, May 15-16
After four decades, refinements to the gold standard of bypass continue as new insights emerge
Why definitive surgical closure is the gold standard, and new ways to make it possible
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches