Advancements are expanding applications and improving accuracy and patient experience
Ever since 1983, when Cleveland Clinic erected a building designed to house its first magnetic resonance imaging (MRI) scanner, it has been exploring new clinical applications for MRI. Some of the most important gains have been made in cardiac MRI, or CMR.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic is now one of the highest-volume CMR centers in the country, conducting over 4,000 scans a year on two dedicated cardiac MRI scanners. Consult QD caught up with Deborah Kwon, MD, Director of Cardiac MRI at Cleveland Clinic, to talk about recent and emerging developments in the field. Seven of them are briefly recapped below.
Cleveland Clinic is using an acceleration technique called compressed sense to perform CMR scans in a more efficient manner. Whereas a typical CMR scan to evaluate cardiac function and myocardial fibrosis/viability usually takes 45 to 60 minutes to complete, myocardial function and tissue characterization MRI studies are typically completed in 30 minutes at Cleveland Clinic using compressed sense.
“Compressed sense is based on the understanding that there is redundant information in signal acquisition,” explains Dr. Kwon. “This technique enables the acquisition of undersampled data, specialized signal processing and image reconstruction to provide high-quality images. To the eye, images acquired using compressed sense look almost identical to images acquired conventionally.” The brief video below shows short-axis image acquisition using compressed sense.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_plmdljib/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Patients who have trouble holding their breath can benefit from another new development — a CMR technique that gates cine acquisition with respiratory bellows to allow free breathing during cine image acquisition. In this technique, the signal is triggered by the motion of the diaphragm as well as the heart. “The scans take slightly longer to perform, but this technique has yielded very nice image quality,” Dr. Kwon observes. “And the ability to perform free-breathing cine imaging can be particularly useful for patients who have trouble performing adequate breath holds, which is frequently the case in those with congestive heart failure.” The brief video below shows free-breathing, non-breah-hold short-axis cine acquisition using respiratory bellows gating technique in a patient with constrictive pericarditis who had trouble performing good breath-holds for traditional cine acquisition.
Advertisement
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_st2pw29q/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
To overcome artifact-related limitations of CMR in patients with pacemakers and implantable cardioverter-defibrillators (ICDs), Cleveland Clinic utilizes an image optimization protocol that uses a wideband imaging technique to minimize artifacts seen on late gadolinium enhancement (LGE) imaging (Figure 1).
“With this technique, we get adequate images on about 70% to 80% of patients with ICDs, even when the devices are not MRI-compatible,” says Dr. Kwon. In the remaining 20% to 30%, close proximity of the ICD to the heart results in significant artifact that obscures a substantial percentage of the heart, which cannot be minimized.
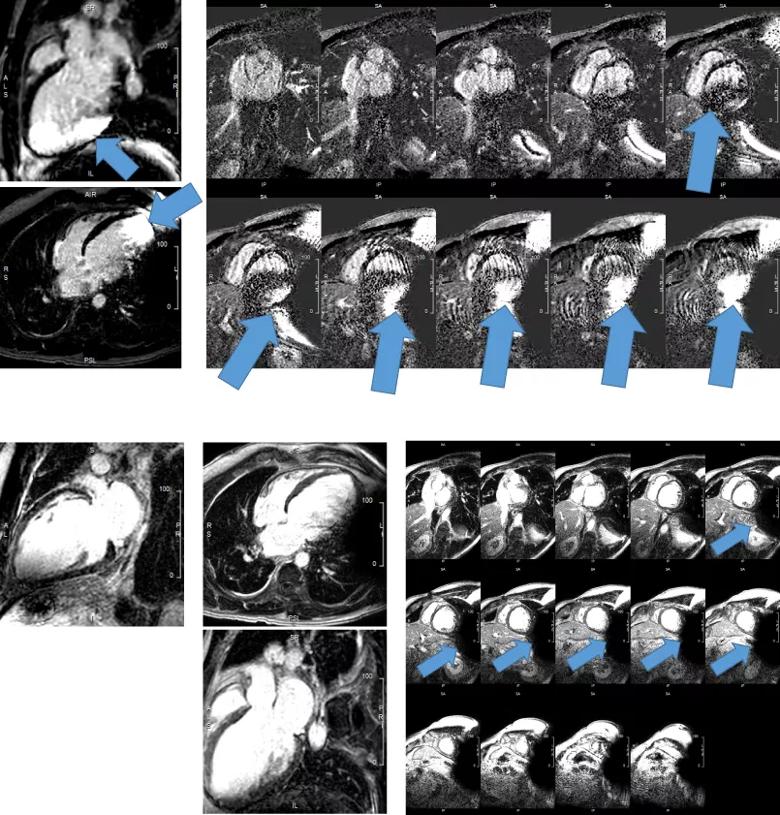
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/79b88752-f4aa-49b0-aa56-7fa21df56246/Revised-Figure-1-Stack_jpg)
Figure 1. (Top) LGE images in a patient with a subcutaneous ICD without wideband phase-sensitive inversion recovery (PSIR) technique. (Bottom) LGE images in the same patient using wideband PSIR technique with a frequency offset of 750 Hz, with resulting artifact minimization.
Fast strain-encoded (SENC) CMR imaging (fast-SENC) is a novel technique that enables assessment of cardiac contractility in a single heartbeat (Figure 2). This technique can identify diseases of the myocardium, including heart failure with preserved ejection fraction and myocardial ischemia, and has promising utility for screening patients in cardio-oncology clinics. The utility of fast-SENC is currently being assessed at Cleveland Clinic for patients with significant valve disease.
“Fast-SENC has demonstrated superior reproducibility for assessing segmental strain,” says Dr. Kwon. She adds that its superior reproducibility of assessing segmental strain results in more accurate assessment of strain than is achieved with other forms of CMR-based strain assessment or with echocardiography.
“Some segments of the myocardium may have abnormal contractility, while other segments may become hypercontractile to compensate,” Dr. Kwon explains. “Therefore, averaging the strain of all segments to provide a global strain value may not be sensitive enough to discern underlying disease. Calculating the number of segments with abnormal strain may provide a more sensitive technique for identifying subclinical myocardial disease. But this requires a technique that provides accurate and reliable segmental measurements. Fast-SENC holds promise for identifying patients early in their myocardial disease trajectory who are at risk for declining contractility over time and may benefit from early therapeutic intervention.”
Advertisement
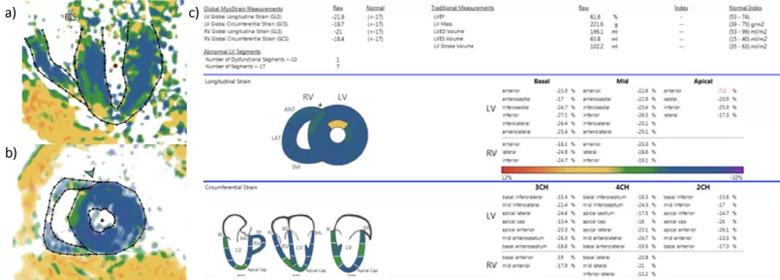
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/990ace81-d16b-4475-9fd8-319f3f6d3952/21-HVI-2187960-Slide4-Inset_jpg)
Figure 2. (a) A four-chamber fast-SENC image. (b) A short-axis fast-SENC image. (c) Segmental and global strain measurements for longitudinal and circumferential strain.
Cleveland Clinic routinely uses parametric mapping with T1 mapping and extracellular volume (ECV) quantification to provide quantitative measurements of the myocardium (Figure 3). The technique can be useful for identifying diffuse fibrosis, myocarditis and cardiac amyloidosis. T2 mapping can be performed to provide quantitative measures of myocardial edema, which can be important for diagnosing active sarcoidosis or other inflammatory myocardial diseases. Quantitative parametric mapping with T1/T2 mapping has lately gained prominence because these techniques were the primary indicators used to characterize COVID-19-related myocarditis in recent literature reports.
“We have been performing T1 mapping routinely since 2014, and it has emerged as an important tool, particularly for identifying early stages of cardiac amyloidosis,” Dr. Kwon notes. “Centers typically rely on LGE imaging to identify patients with cardiac amyloidosis, but LGE assessment can miss amyloidosis in up to 15% of patients who are in the early stages. T1 mapping and ECV quantification provide significantly more sensitive measures to identify more subtle and diffuse abnormalities in myocardial tissue. T1 and T2 mapping may also be important for identifying early stages of myocarditis secondary to viral illness or in cancer patients undergoing chemotherapy.”
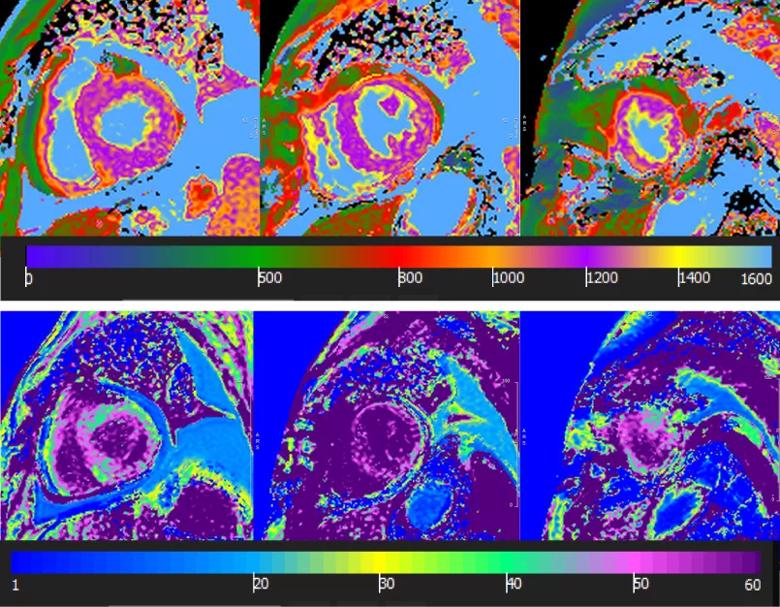
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/91d00323-d287-4ddf-bff0-f6ac94f03aa8/21-HVI-2187960-Slide5-Inset_jpg)
Figure 3. Quantitative parametric mapping. (Top) Precontrast T1 mapping in a patient with cardiac amyloidosis. (Bottom) Mapping with extracellular volume quantification.
Cardiac MR fingerprinting (cMRF) has recently emerged as a novel and robust quantitative parametric technique that enables quantification of T1 and T2 values in a single breath-hold (Figure 4). In addition to streamlining protocols and making scanning more efficient, cMRF may provide further tissue characterization beyond T1/T2 measures, such as fat fraction, perfusion, diffusion, T2* and the ability to quantify ECV without gadolinium-based contrast agents. cMRF is still in the research stage, but Dr. Kwon expects to implement this technique in clinical scans at Cleveland Clinic later this year.
Advertisement
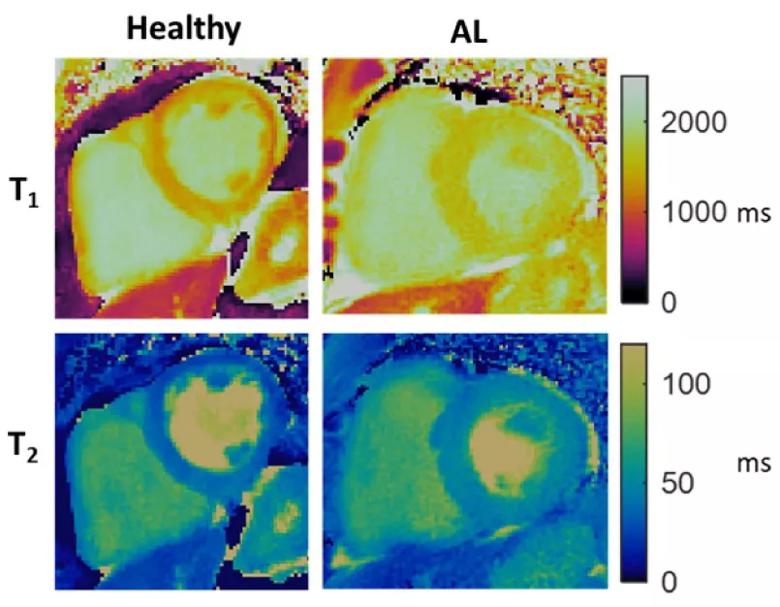
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5cbc8526-c84c-4698-bd86-fb88d4939275/21-HVI-2187960-Slide6-Inset_jpg)
Figure 4. Cardiac MRF for characterization of a healthy volunteer relative to a patient with AL amyloidosis (AL).
To conduct MRI stress testing, an exercise ergometer made specifically for use in MRI scanners can be loaded onto the scanner table. Resting images are acquired, after which the patient cycles for up to 10 minutes with his or her chest inside the magnet. Cine imaging and strain imaging can then be acquired while the patient is still cycling to assess heart function at rest and under stress (Figure 5).
“The biggest hurdle has been imaging patients while exercising due to increased respiratory rate, increased heart rate and increased body motion from cycling — these are all obstacles to acquiring good CMR images,” Dr. Kwon explains. “By using compressed sense and shortening breath-holds to 3 seconds, we have been able to address some of these challenges, but image optimization is still ongoing.”
The test is being developed for use in asymptomatic patients with valvular heart disease and heart failure with preserved ejection fraction, in whom changes are likely visible at submaximal exercise levels. “It is more sensitive for patients with early signs of myocardial disease and will be useful when we are unsure whether a patient should have surgery,” she says.
The imaging protocol during exercise is being refined on healthy volunteers with the goal of conducting research studies to determine clinical feasibility and utility.
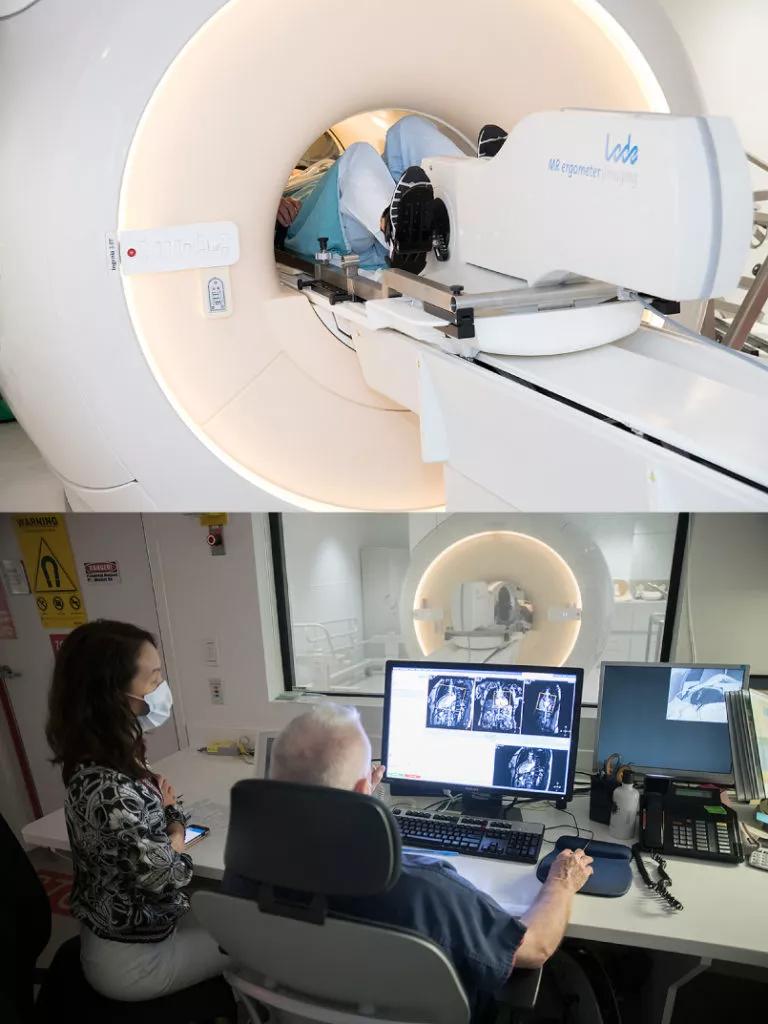
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e896fc32-1c1d-4326-beb9-1927fad92c28/21-HVI-2187960-exercise-ergometer-in-MRI-scanner_Inset-768x1024_jpg)
Figure 5. Photos of a volunteer using the ergometer in an MRI scanner while Dr. Kwon and a colleague observe the resulting images on a monitor.
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon
How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR
Optimal management requires an experienced center