Serial strain assessments show sustained favorable impacts on LV systolic function and LA function
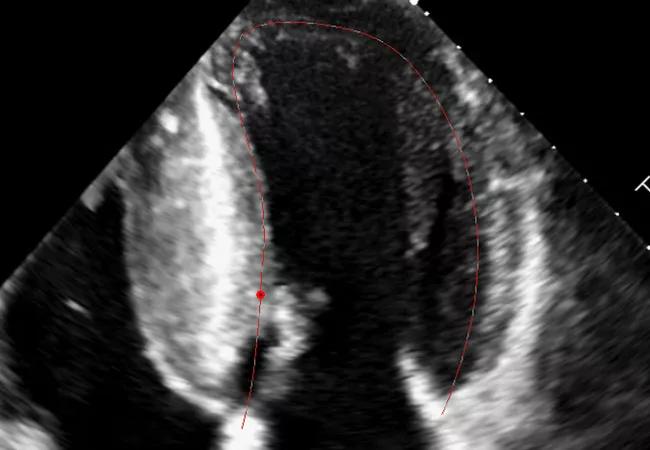
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/79cfccb6-6d4c-49aa-aada-f3a7146d74e5/17-HRT-4638-Strain-HOCM-CQD-Feat_jpg)
echocardiogram showing strain imaging assessment
Treatment with mavacamten provides sustained improvement in left ventricular global longitudinal strain (LV-GLS) in patients with severe symptomatic obstructive hypertrophic cardiomyopathy (HCM) with no detrimental effect on right ventricular (RV) systolic function. It also results in sustained improvement in left atrial (LA) volume index and LA strain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So conclude two subanalyses of the pivotal phase 3 VALOR-HCM study of mavacamten through 56 weeks. Both were presented at the European Society of Cardiology’s ESC Congress 2024 and simultaneously published online — the LV strain study in Circulation: Cardiovascular Imaging and the LA strain study in JACC: Cardiovascular Imaging.
The analyses suggest that mavacamten has sustained favorable impacts on regional LV systolic function as well as LA remodeling and LA function. “Whether these serial imaging findings have longer-term prognostic implications still needs to be determined,” says Milind Desai, MD, MBA, Director of Cleveland Clinic’s Hypertrophic Cardiomyopathy Center and first author of both studies.
Conducted at Cleveland Clinic and 19 other U.S. sites, VALOR-HCM is a double-blind, randomized, placebo-controlled crossover trial evaluating mavacamten’s effects in patients with obstructive HCM. All 112 participants had severe symptoms despite maximally tolerated medical therapy and had been referred for septal reduction therapy (SRT).
Randomization was to 5 mg/day of oral mavacamten or placebo, with titration of the dosage up or down based on echocardiographic assessment of LV outflow tract (LVOT) gradients and LV ejection fraction (LVEF). The primary endpoint was a composite of either a decision to proceed with SRT or continued guideline-based eligibility for SRT. At 16 weeks, patients initially randomized to placebo were crossed over to mavacamten.
In 2022, 16-week results from the VALOR-HCM showed that significantly fewer patients in the mavacamten group than in the placebo group met the primary endpoint. This formed the basis for mavacamtem’s FDA approval that year, making the cardiac myosin inhibitor the first drug therapy formally indicated for adults with symptomatic obstructive HCM. Those results were sustained in subsequent planned 32- and 56-week analyses.
Advertisement
Previous reports from VALOR-HCM have demonstrated that mavacamten improves LVOT gradient, quality of life, symptom burden and physical functioning in patients with symptomatic obstructive HCM, in addition to the primary objective of reducing the need for SRT.
“Mavacamten has also been shown to result in favorable cardiac remodeling, including improving LV diastolic function, LA volume index and biomarkers such as N-terminal pro b-type natriuretic peptide and troponin T,” says co-investigator Zoran Popovic, MD, PhD, a cardiologist in Cleveland Clinic’s Section of Cardiovascular Imaging. “However, its impact on sensitive measures of regional myocardial function such as GLS has been unknown, as has its effect on LA function. These analyses were undertaken to address those knowledge gaps.”
LV-GLS has been used in small observational studies to document important temporal changes in cardiac structure and function in patients who have undergone surgical myectomy. In the broader HCM population, other observational reports suggest that LV-GLS impairment is a significant prognostic factor for future clinical events, such as sudden cardiac death, heart failure and ventricular arrhythmia.
The VALOR-HCM investigators measured LV and RV end-systolic and end-diastolic volumes indexed to body surface area, as well as LVOT gradients and intraventricular septal thickness and LVEF. Vendor-neutral post-processing software was used for the blinded, offline LV- and RV-GLS assessment.
Regions of interest were automatically traced with the post-processing software and corrected manually if needed. Peak LV-GLS was determined with nonforeshortened apical (four-, three- and two-chamber) views. RV four-chamber and free wall strain were calculated with RV focused four-chamber view.
Advertisement
Principal findings from the analysis included the following:
From a hemodynamic standpoint, the LA plays a key part in modulating LV diastolic filling through three basic functions that correspond with LA strain assessment: a reservoir function (i.e., collection of pulmonary venous return during ventricular systole), a conduit function (i.e., passage of blood to the LV during early diastole) and a contractile booster pump function (i.e., augmentation of ventricular filling during late diastole).
Advertisement
Echocardiographic LA strain has been used to characterize diastolic dysfunction and to stratify risk of atrial fibrillation (AF) among patients with HCM. Myectomy has been shown to improve LA dimensions and diastolic function in patients with obstructive HCM, but few investigations have assessed changes in LA phasic function. Mavacamten has likewise been shown to lead to favorable cardiac remodeling, including improvements in LA volume index and diastolic function, but its effect on serial changes in LA function has not been evaluated.
As part of the serial echocardiographic assessments in VALOR-HCM, investigators measured LA strain in terms of three components — conduit, reservoir and contraction strain — using the same vendor-neutral post-processing software as for LV strain.
Principal findings were as follows:
Advertisement
“This is one of the first prospective investigations to show early and enduring improvements in LA strain measures, in addition to LA volume index, in patients with obstructive HCM treated with a cardiac myosin inhibitor,” Dr. Popovic notes.
“We found that baseline LV-GLS and RV strain and baseline LA volume index and LA strain were worse than normal reference values in the VALOR-HCM population despite hypercontractile LVEF and preserved RV systolic function,” Dr. Desai says. “This is consistent with the advanced phenotype of obstructive HCM.
“Mavacamten therapy was associated with sustained and serial improvements in LV-GLS and LA strain through 56 weeks,” he continues, “which suggests enduring favorable impact on regional LV systolic function and favorable LA remodeling. This was achieved with no significant harmful effect on RV volumes or systolic function.”
The investigators note that abnormal baseline LV-GLS may have long-term incremental prognostic value by identifying an HCM phenotype associated with higher risk of cardiac events, such as a massively hypertrophied LV or higher fibrosis burden.
“It makes intuitive sense that LV-GLS and LA hemodynamics would improve as a result of the changes in hemodynamic load associated with mavacamten’s positive impact on LVOT obstruction,” Dr. Desai observes. “But the strain values did not normalize at week 56.”
That finding, along with the absence of strain improvements in patients with mavacamten interruption due to transient LVEF reduction, leaves the researchers with several remaining questions about cardiac myosin inhibitor therapy:
“We intend to continue our research to address these issues in an effort to refine the utility of this new class of medical therapy for obstructive HCM,” Dr. Desai concludes.
“On the face of it, these studies highlight what strain can teach us about mavacamten in patients with HCM,” says Patrick Collier, MD, PhD, a Cleveland Clinic cardiovascular imaging specialist who was not involved in the study. “But there is a double benefit here, along with potential breakthroughs for the field of echocardiography and a wider cohort of patients, when one considers the reverse: What additional insights can such novel therapeutics teach us about strain? This additional benefit is underscored by the fact that that they impact outflow tract obstruction, hypertrophy, mitral regurgitation, fibrosis and atrial remodeling — for which strain is a composite surrogate. Moreover, their use mandates close and careful serial echocardiography studies to be performed in echo laboratories around the world.”
Advertisement
End-of-treatment VALOR-HCM analyses reassure on use in women, suggest disease-modifying potential
Cardiac imaging substudy is the latest paper originating from the VANISH trial
Vigilance for symptom emergence matters, a large 20-year analysis reveals
Phase 3 ODYSSEY-HCM trial of mavacamten leaves lingering questions about potential broader use
5% of flagged ECGs in real-world study were from patients with previously undiagnosed HCM
High composite score in myectomy specimens signals worse prognosis
Few patients report left ventricular dysfunction or heart failure after one year
Avoidance of septal reduction therapy continues while LVEF dysfunction remains infrequent