Study finds important discrepancies among modalities and techniques
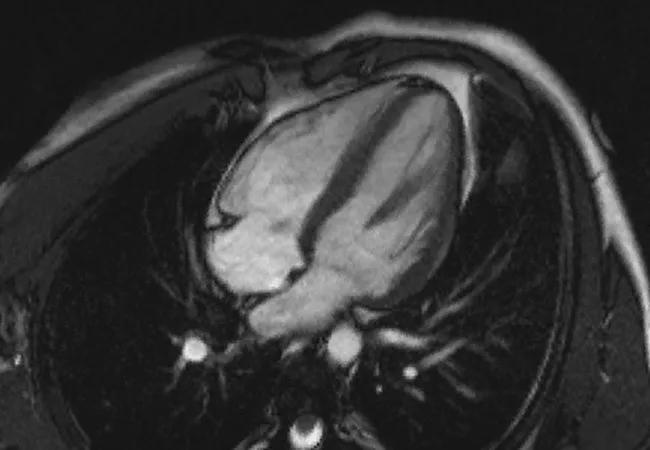
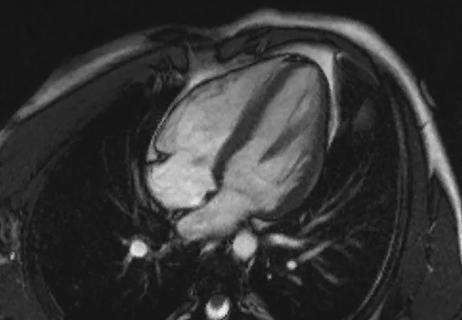
For patients with hypertrophic obstructive cardiomyopathy (HOCM), optimal surgical planning to relieve left ventricular outflow tract obstruction (LVOTO) during surgical myectomy demands precise morphological assessment. However, data on concurrence between various types of multimodality imaging to provide such assessment are scarce. Now Cleveland Clinic researchers have published prospective data on this question, outlining which measurements are best for specific purposes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“It’s helpful to recognize the strengths and drawbacks of the various techniques that allow different types of measurements in HOCM patients undergoing myectomy because these measurements are not interchangeable,” says Milind Desai, MD, MBA, senior author of the newly published research (Am J Cardiol. 2024;227:48-56) and Medical Director of Cleveland Clinic’s Center for Hypertrophic Cardiomyopathy.
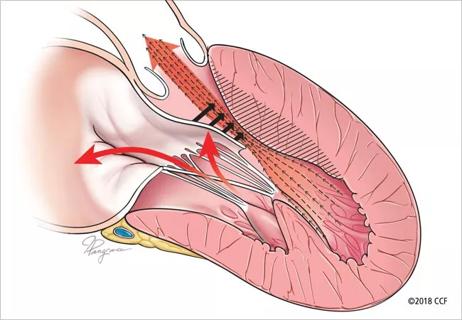
“It’s increasingly clear that the causes of LVOTO are not always limited to a hypertrophied interventricular septum,” adds co-author Nicholas Smedira, MD, MBA, Surgical Director of the Center for Hypertrophic Cardiomyopathy. “Elongated mitral valve leaflets and other structural abnormalities of the mitral valve may contribute too, and they often require adjustment of the surgical approach to relieving LVOTO.”
While surface echocardiography is well suited to helping determine whether a patient is a candidate for surgical myectomy, transesophageal echo (TEE) and cardiac magnetic resonance imaging (CMR) are often needed to make the precise septal and mitral leaflet measurements for determining how much septal debulking and mitral valve repair are required to address LVOTO.
Dr. Desai notes that CMR, given its superior spatial resolution, is recognized as the gold standard for septal measurements, whereas intraoperative TEE is the go-to modality for intraoperative assessment and guidance. Several TEE techniques are also used to gauge mitral leaflet length and morphology. “However,” he adds, “the accuracy of different intraoperative TEE techniques for septal and mitral valve measurements is not well defined in this setting, nor is their correlation with CMR. We undertook this investigation to compare interventricular septal thickness and mitral leaflet lengths as measured by intraoperative TEE techniques with preoperative CMR measurements.”
Advertisement
The researchers prospectively studied 50 adults with HOCM who underwent surgical myectomy for symptomatic LVOTO in 2018 or 2019. All patients underwent imaging with preoperative CMR and intraoperative TEE. The cohort was 44% male and had a mean (±SD) age of 59 ± 12 years.
Maximal basal, mid and distal anteroseptum and inferoseptum measurements were taken using multiplanar 3D reconstruction on TEE and using short-axis imaging on preoperative CMR. Maximal wall thickness was categorized as mild (≤18 mm), moderate (18-25 mm) or severe (≥25 mm) based on CMR measurement.
Mitral valve leaflet lengths were measured by preoperative CMR and intraoperative 2D TEE, zoom 3D TEE and automatic mitral valve quantification (AMVQ).
“Our study is novel in the use of multiple intraoperative TEE techniques (including 2D and 3D multiplanar reconstruction) to correlate septal and mitral measurements with CMR,” the authors wrote in their study report.
Key findings were as follows:
Advertisement
“There are two main takeaways from our results,” Dr. Desai says. “One is that intraoperative 3D TEE with multiplanar reconstruction tends to overestimate septal wall thickness compared with preprocedural CMR, particularly in patients with milder hypertrophy. The other is that mitral leaflet length measurements vary considerably between 3D TEE and CMR and also among the different TEE techniques. It is therefore not recommended to extrapolate from one technique to another.”
Dr. Smedira notes that the findings on septal wall thickness should prompt particular caution. “Our findings suggest that sole reliance on intraoperative 3D TEE to guide septal resection may lead to resection of too much muscle and potential harm,” he says. “This is especially the case in the setting of mild septal thickness and primary mitral leaflet abnormality, where excessive resection could lead to a ventricular septal defect and/or heart block.”
The authors conclude that their findings lend support to current mainstays of anatomic assessment in the setting of HOCM treated with surgical myectomy. “A reliance on gold-standard techniques to respectively measure septal thickness (CMR) and mitral valve morphology (3D TEE multiplanar reconstruction) is important as part of preoperative and intraoperative planning,” they wrote in their study report.
“This study further supports the long-held contention of cardiac imagers that different cardiac imaging modalities have uniquely specific value and indications,” adds Richard Grimm, DO, Director of the Echocardiography Laboratory at Cleveland Clinic, who was not involved in the study. “CMR demonstrated its diagnostic value for measuring septal thickness, and TEE showed its value for evaluating mitral valve morphology, motion and competency. In the context of myectomy for HOCM, CMR’s high spatial resolution is valued for surgical guidance, whereas the high combined spatial and temporal resolution provided by TEE enables optimal analysis and definition of valve anatomy and motion/function to assure valve competency following the surgery.”
Advertisement
Advertisement

End-of-treatment VALOR-HCM analyses reassure on use in women, suggest disease-modifying potential

Cardiac imaging substudy is the latest paper originating from the VANISH trial

Vigilance for symptom emergence matters, a large 20-year analysis reveals

Phase 3 ODYSSEY-HCM trial of mavacamten leaves lingering questions about potential broader use

5% of flagged ECGs in real-world study were from patients with previously undiagnosed HCM

High composite score in myectomy specimens signals worse prognosis
Few patients report left ventricular dysfunction or heart failure after one year
Avoidance of septal reduction therapy continues while LVEF dysfunction remains infrequent