A close-up look at outcomes for the most common to rarest procedures
Expanded public reporting of procedural outcomes has been one of the most positive developments in the cardiovascular and thoracic specialties over the past decade. Public reporting focuses care teams on outcomes that ultimately matter most to patients and their families: whether and how long they survive, and how well their quality of life is maintained or improved.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Yet as helpful as public reporting may be in continually driving care quality, providers must take care not to let it turn outcomes analysis into a purely abstract exercise. Numbers and percentages alone may dictate Society of Thoracic Surgeons (STS) star ratings, but they do not properly capture what the underlying procedures mean to individual patients.
To keep focused on the impact of overall surgical outcomes at this patient level, staff in Cleveland Clinic’s Miller Family Heart, Vascular & Thoracic Institute did an extra round of number crunching early this year when looking back at their adult cardiac surgery and thoracic surgery volumes and outcomes in 2019 and the preceding years.
As illustrated in the graph below, Cleveland Clinic’s in-hospital mortality rates for these major surgical categories have shown a cumulative and largely steady decline over the past 13 years. For adult cardiac surgery, mortality has been slashed by two-thirds, from 3.3% in 2007 to 1.1% in 2019. Thoracic surgery mortality dropped even further over the same period, from 4.4% to 1.2%.
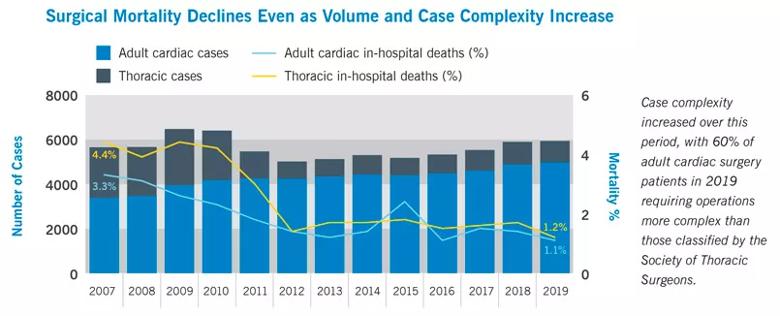
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/17512fb1-76d0-4353-bdfd-1626f3fd73ce/20-HVI-1874809-Close-Up-Surgical-Outcomes-CQD-Inset-2_jpg)
These improvements in mortality were achieved even as surgical volumes steadily increased in the case of adult cardiac surgery and even as case complexity increased for both thoracic and adult cardiac procedures. In fact, 60% of adult cardiac surgery patients in 2019 required operations more complex than those classified by STS.
The additional number crunching mentioned above focused on how these continuing improvements in mortality translated in terms of actual patient lives saved, and calculations showed that the changes in mortality saved approximately 1,500 lives in the 10 years from 2010 through 2019 alone.
Advertisement
“This is a humbling number to consider, and it helps affirm for all caregivers why we chose the calling we did,” says Lars Svensson, MD, PhD, Chair of the Heart, Vascular & Thoracic Institute. “Over time, we have also reduced rates of wound infection, renal failure, GI complications and, for some procedures, stroke. These improvements translate to better quality of life — in addition to longer life — for countless patients.”
A sizeable share of the operations included in these data are the mainstays of adult cardiac surgery and thoracic surgery for which the STS evaluates hospitals and health systems with its star rating system. In the latest reporting periods for the STS Adult Cardiac Surgery Database and General Thoracic Surgery Database, Cleveland Clinic received the highest (three-star) composite quality rating in all categories assessed, as detailed in the table below.
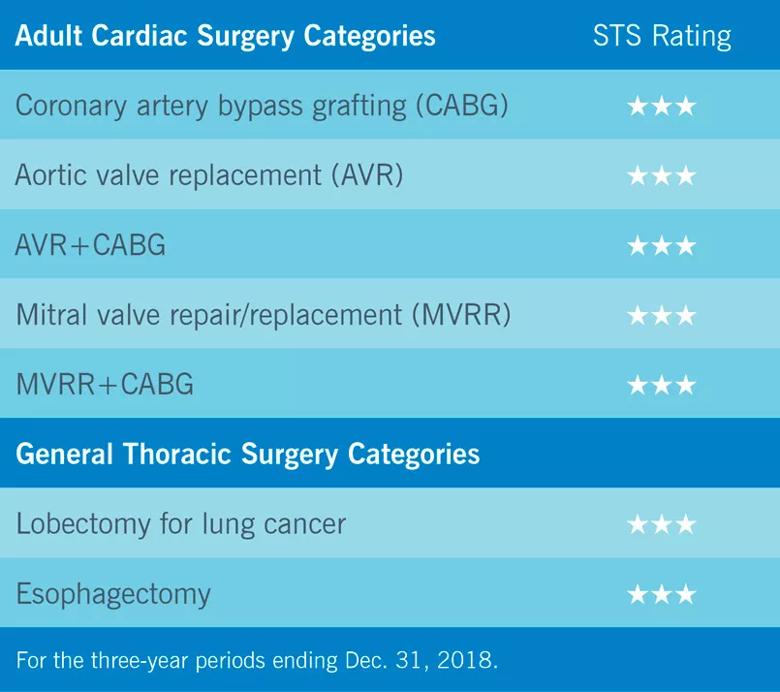
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/11645cfd-dc2d-4fd0-83c1-72574f907b8a/20-HVI-1874809-Close-Up-Surgical-Outcomes-CQD-Inset-1_jpg)
At the same time, these mainstay operations represent less than half of the overall adult cardiac surgery and thoracic surgery procedures performed at Cleveland Clinic. As a result, most of the surgeries included in the mortality graph above are procedures for which the STS doesn’t report risk-adjusted benchmark rates, often because of relative rarity or substantial complexity.
For example, 1,129 of the adult cardiac surgeries performed at Cleveland Clinic in 2019 — over 21% of the total — were reoperations. Other operations in the cardiothoracic surgical mix are uncommon procedures not offered widely elsewhere and requiring volume-based expertise. The rest of this article profiles a small sampling of such operations — and the difference that Cleveland Clinic’s expertise can make for individual patients needing these procedures.
Advertisement
While efforts to repair the aortic valve date back several decades, the breakthrough in valve-sparing aortic root aneurysm repair came in the early 1990s with cases first reported by Tirone David, MD, who completed his general surgery residency at Cleveland Clinic.
The so-called David reimplantation procedure involves mobilizing the aortic valve, inserting it within a polyester tube graft, attaching coronary buttons, and then replacing the aneurysmal root and ascending aorta. The operation demonstrated good durability, but a number of complications — including fistulas, mitral valve tears and aortic valve leakage over time — prompted efforts to further refine the technique.
Among those leading these efforts was Cleveland Clinic’s Lars Svensson, MD, PhD, who visited Dr. David later in the 1990s to learn the procedure. Dr. Svensson soon began to develop several modifications of the David operation, including the following:
These modifications were described by Dr. Svensson in a 2003 publication (Ann Thorac Surg. 2003;76:1751-1753), and the modified operation has been called the Svensson or LGS reimplantation procedure. It had been performed in over 990 Cleveland Clinic patients through the end of 2019, giving Cleveland Clinic the world’s largest experience in aortic root replacement with valve reimplantation.
Advertisement
“About 90% of those cases have been elective operations, and the mortality rate in these elective cases is 0.14%,” Dr. Svensson notes. “Mortality in emergency and urgent cases has been low as well, at 3.0%.”
Despite the growth of valve-sparing aortic root replacement at Cleveland Clinic, where it is done by a number of staff cardiothoracic surgeons, the operation remains a relative rarity in much of the rest of the U.S., with only two other centers performing the procedure on a regular basis.
Dr. Svensson says that while late outcomes of valve-sparing aortic root replacement have not been thoroughly examined, recent analysis of such outcomes among Cleveland Clinic patients suggests that earlier intervention promises equal or better outcomes than watchful waiting. These data have been submitted for publication, he notes.
Pericardiectomy has long been viewed as a high-risk operation for which a limited anterior “phrenic to phrenic” off-pump approach has been advocated. Surgeons at Cleveland Clinic have developed a systematic approach focusing on radical resection and routine use of cardiopulmonary bypass in this procedure for patients with constrictive or chronic recurrent pericarditis.
“Anterior resection from phrenic nerve to phrenic nerve via a thoracotomy approach achieves symptom improvement, but some patients still have progressive constriction of the remaining pericardium that requires redo pericardiectomy,” says Cleveland Clinic cardiothoracic surgeon Shinya Unai, MD. “Recent evidence demonstrates superior survival and functional outcome with a complete pericardiectomy.”
Advertisement
As a result, since 2008 Cleveland Clinic surgeons have switched to an approach performed via median sternotomy with routine use of cardiopulmonary bypass to achieve radical resection of the pericardium and “pedicalization” of both phrenic nerves. “Pedicalization involves completely removing the pericardium from the phrenic nerve, leaving a small amount of fat,” Dr. Unai explains.
In a recent review of radical pericardiectomy for pericardial diseases (Curr Cardiol Rep. 2019 Feb 12;21:6), he and colleagues reported Cleveland Clinic’s experience with pericardiectomy in 601 patients from 1977 to 2013. Overall in-hospital mortality was 6%, with mortality for patients with idiopathic pericarditis as low as 1.2% in operations performed since 2000.
“Even with aggressive resection and the use of cardiopulmonary bypass, the rate of reoperation for bleeding was only 3.8%,” Dr. Unai notes. He adds that advances in postoperative management kept requirements for intra-aortic balloon pump and extracorporeal membrane oxygenation at 2.6% and 1.7%, respectively.
“Short-term outcomes of pericardiectomy have improved substantially at experienced centers that select patients carefully,” Dr. Unai says. “We favor aggressive removal of the entire pericardium, particularly for patients with relapsing pericarditis, as it doesn’t increase operative risk.” He and colleagues recently presented Cleveland Clinic data showing that long-term survival is improved with this approach as opposed to performing a partial resection (Barrios et al., American Association for Thoracic Surgery annual meeting 2019, abstract 202).
Cleveland Clinic thoracic surgeons were among the earliest adopters of robotic technology for general thoracic surgery. Today they use video-assisted thoracic surgery (VATS) or robotic assistance for the following procedures, among others:
“Taking advantage of this technology is critical to our goal of treating disease with as little collateral injury as possible,” says Sudish Murthy, MD, PhD, Section Head of General Thoracic Surgery. “Patients can reap the benefits of outcomes equivalent to those with open surgery but with less treatment-associated morbidity.”
Very small incisions are needed for robotically assisted surgeries, he notes, and deep tissues can gently be pushed out of the way with the robotic arms instead of cut, causing less internal damage. This results in less blood loss and reduced postoperative pain. Scarring is also minimized, which is an important advantage if an additional surgery is needed.
“We believe our judicious use of minimally invasive VATS and robotically assisted techniques is an important contributing factor to our consistent three-star composite quality ratings from STS for lung cancer and esophagectomy,” says Dr. Murthy.
Moreover, patient recovery times are shorter with robotic and VATS procedures, with fewer days spent in the hospital. This is borne out by Cleveland Clinic’s steadily declining median length of stay (LOS) for lobectomy patients, which was reduced to 3 days in 2018. Robotic and VATS procedures have driven the decline, as they were associated with median LOS values 1 to 2 days shorter than their open-procedure counterparts in 2018 across various types of lobectomies.
“We are increasing our use of minimally invasive techniques for more complex operations while simultaneously instituting perioperative protocols designed to hasten recovery,” notes thoracic surgeon Usman Ahmad, MD. “We are finding that such initiatives allow our patients to resume their normal activities more quickly without compromising safety.”
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more