Studies find mTOR inhibitor may play key role in treating Hurthle cell carcinoma
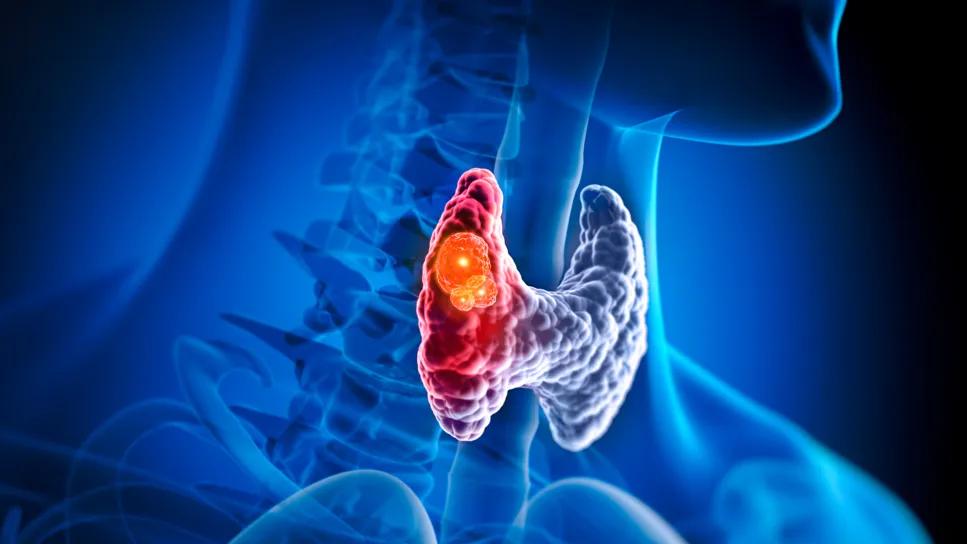
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0a7b4766-f546-4662-a0cd-90fb77b547d5/hurthle-cell-carcinoma-2169560490)
Hurthle cell carcinoma
Hurthle cell carcinoma (HCC) is a rare type of thyroid cancer that is not responsive to standard therapies like radioactive iodine. When the disease spreads, it becomes extremely difficult to treat. As with many rare cancers, HCC has historically been understudied.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Clinical investigators have been working to change that.
Until recently, little was known about the molecular makeup of HCC. In fact, just a few years ago, HCC was mistakenly classified as a subset of follicular thyroid cancer. Timothy Chan, MD, PhD, and Jeffrey Knauf, PhD, were part of a team that dispelled this misconception.
Several years ago, the pair were part of a research team that published the first genomic analysis of HCC, demonstrating its unique mutations. They are now seeking to make these mutations actionable as therapeutic targets.
HCC is a unique type of cancer that has limited preclinical models. The researchers have recently developed seven new Hurthle cell patient-derived xenograft models and plan to develop 15-20 additional preclinical models to explore potential therapeutic targets.
Working with the Head and Neck Oncology division at Cleveland Clinic, the researchers set out to:
Earlier studies indicated that mTOR signaling is altered in HCC, suggesting this pathway as potential therapeutic targets. One small clinical trial found that combining the mTOR inhibitor everolimus with the kinase inhibitor sorafenib significantly improved progression-free survival over sorafenib alone.
The researchers’ goal is to move into larger clinical trials to validate mTOR inhibitors are as a viable treatment for HCC. “This study initiated much planning around how to demonstrate that mTOR inhibitors were targeting something important,” says Dr. Chan. “If we can show that HCC with mTOR mutations respond well to mTOR inhibitors, it could support a future FDA indication.”
Advertisement
“We’re trying to understand the dependency on the mTOR pathway using these novel preclinical models we’ve been building,” says Dr. Knauf. “Through this work, we aim to understand the mechanisms of resistance to the drug, and understand other genomics so that we can better assess which patients will respond to treatment.”
The researchers also sought to assess the effect that HCC had on the immune system and if that had any bearing on therapies being used. To do so, they performed RNA sequencing on HCC tumors to understand the immune microenvironment. The data revealed that the microenvironment in HCC is often low in immune cells. Tumors that had a global loss of heterozygosity (LOH) had very low levels of immune infiltration, which may indicate a low probability of responding to immunotherapy. Notably, mTOR inhibitors work by blocking the mTOR pathway, which can be essential for tumor growth and survival, whereas immunotherapies work by activating the immune system to recognize the tumor as foreign.
As one of the few cancer centers with experience treating HCC, Cleveland Clinic Cancer Institute brought together a multidisciplinary team of surgeons, thyroid specialists and cancer investigators to focus on this rare cancer. “HCC behaves differently on a molecular level in comparison other thyroid cancers and must be treated differently,” says Dr. Chan.
Currently, mTOR inhibitor combination therapy is being further studied in a phase 2 trial. At the same time, the researchers are working to develop more novel therapies.
Advertisement
Advertisement
Advertisement
Dynamic risk assessment may aid clinicians in helping support informed treatment decisions
A new study indicates that the combined approaches can be performed without mortality and with acceptable morbidity
New research provides clinical insight into prognostic factors
Struma ovarii can give rise to uncommon malignancy
Only 33% of patients have long-term improvement after treatment
OMT may be right for some with Graves’ eye disease
Radiofrequency ablation significantly reduces symptom severity, shrinks nodules
Timing and type of side effects differ greatly from chemotherapy