The rare condition can cause structural damage if untreated
Written by Malek H. Bouzaher, MD, Suat Kilic, MD and Samantha Anne, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Note: This article is reprinted from the Cleveland Clinic Journal of Medicine (2023;90[5]:279-281)
After having an abnormal ear examination and a failed hearing screening at her well-child visit with her pediatrician, a 15-year-old female presented for an audiogram, which revealed a left-sided conductive hearing loss. The patient had a history of recurrent acute otitis media of both ears requiring two sets of pressure-equalization tubes at ages 2 and 4. There was no family history of hearing loss and no recent history of head or auricular trauma.
Examination in the office was normal on the right side but demonstrated an atelectatic tympanic membrane on the left with a retraction pocket and keratin debris posterosuperiorly. Facial nerve function was intact bilaterally.
Computed tomography of the temporal bones demonstrated a left-sided retracted tympanic membrane with soft tissue extending to the long process of the incus, with erosion and demineralization of the ossicle (Figure 1). A retraction cholesteatoma was suspected, which is a type of acquired cholesteatoma that develops with trapping of cholesteatoma within a deep retraction of the tympanic membrane.
She was subsequently taken for tympanoplasty with middle ear exploration. Intraoperatively, cholesteatoma was noted involving the incus and significant erosion. The incus was removed, and the stapes suprastructure was found to be uninvolved and was left intact. She underwent ossicular chain reconstruction with a partial ossicular replacement prosthesis after complete removal of the cholesteatoma. Postoperative audiography demonstrated improvement in hearing thresholds.
Advertisement
The patient continued to be followed for cholesteatoma, with no recurrence of the disease. Cholesteatomas can recur with an overall disease rate of 4.6% and a residual disease rate of 5.4%,1 and therefore these patients should be monitored for residual or recurrent disease.
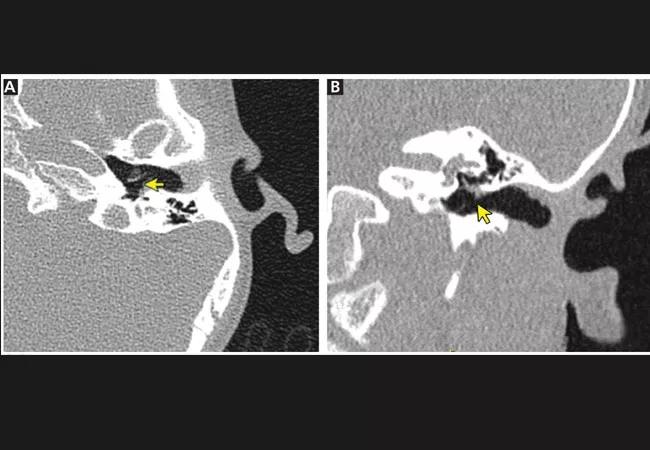
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5c4415e2-fcfb-4766-a2f7-8e2601ee2a1c/23-HNI-4147725-CaseStudy-Cholesteatoma-CQD-hero_650x450-1_jpg)
Figure 1. Computed tomography of the patient’s temporal bone, without contrast. (A) The axial view shows demineralization and erosion of the incus (arrow), and (B) the coronal view shows soft-tissue extension along the length of the incus (arrow).
The term cholesteatoma was first used in a case report in 1838 to describe a ‘‘tumor” thought to be made of cholesterol and fat (chole- for cholesterol, steat- for fat, and –oma for tumor).2 This term continues to be used despite the understanding over time that it is instead a progressively enlarging and destructive lesion composed of keratinizing squamous epithelium.3
Cholesteatoma is considered congenital when presenting as a white mass behind an intact eardrum in a patient with no history of otitis or previous otologic surgery.2,3 Acquired cholesteatoma, localized exclusively in the middle ear, affects children and adults and occurs in three to 15 per 100,000 children and nine to 12.6 per 100,000 adults.2
Acquired cholesteatoma is often seen in patients with a history of eustachian tube dysfunction, recurrent middle ear infections, or previous otologic surgery,4 or with a pearly white or yellowish mass behind the tympanic membrane in the middle ear (Figure 2).5 Cholesteatoma may encroach on or erode nearby structures and become secondarily infected, leading to the onset of symptoms as it expands (Figure 2).5 If left untreated, cholesteatoma may erode through the temporal bone or inner ear, where it can cause a perilymphatic fistula, sensorineural hearing loss, vertigo, cerebrospinal fluid leaks, central nervous system infection, or cranial nerve deficits.5,6
Advertisement
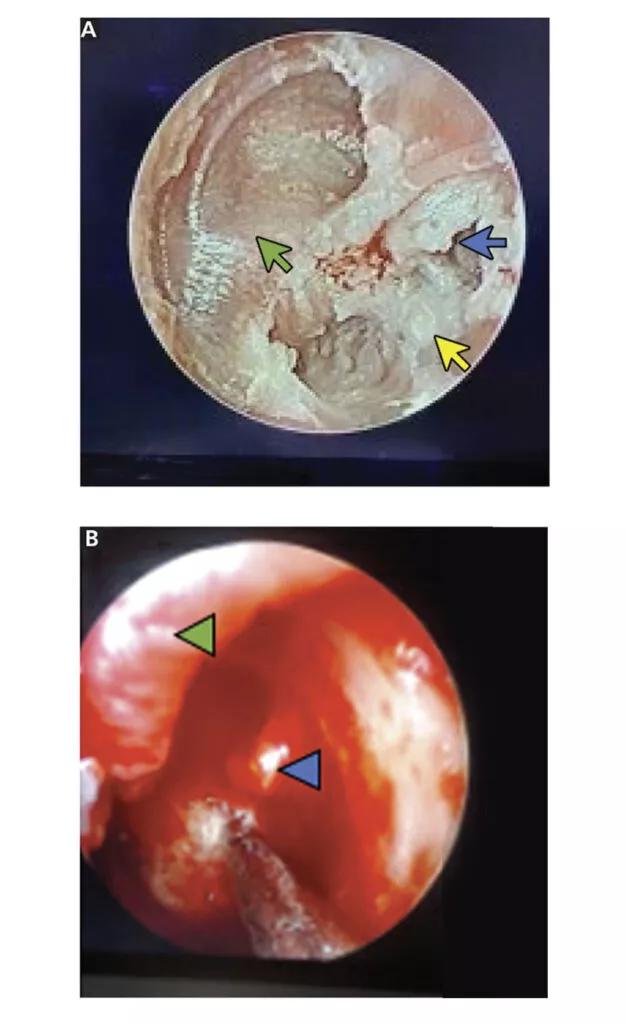
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6966ace8-3565-4355-b3ef-ddc2fab7df39/23-HNI-4147725-CaseStudy-Cholesteatoma-CQD-inset_800x1309-1-626x1024_jpg)
Figure 2. (A) Intraoperative visualization of the patient’s retraction cholesteatoma (yellow arrow) prior to removal, with keratin debris in the posterosuperior quadrant (blue arrow). A small remnant of normal tympanic membrane was noted near the annulus anteriorly (green arrow). (B) After elevation of the tympanic membrane (green arrowhead), the lesion was found to have eroded through the tip of the incus (blue arrowhead).
Hearing loss is one of the most common symptoms of cholesteatoma. It is predominantly conductive in nature and may be due to otorrhea resulting from secondary infection, chronic inflammation leading to edema and granulation tissue formation, or ossicular erosion.6 Rarely, cholesteatoma can cause sensorineural hearing loss if it extends to the inner ear.5,6
Patients with cholesteatoma may classically present with hearing loss in the setting of an apparent ear infection, abnormal appearance of tympanic membrane and middle ear, or an otherwise normal physical examination. The typical conductive hearing loss that occurs with cholesteatoma must be differentiated from sensorineural hearing loss and other causes of conductive hearing loss such as trauma, ossicular discontinuity, and otosclerosis.
Patients with an abnormal examination, a history of recurrent middle ear infections, eustachian tube dysfunction or previous otologic surgery, or patients with symptoms that fail to improve with treatment should be promptly referred to an otolaryngologist for further evaluation and management.
Advertisement
References
Dr. Anne recently presented on pediatric cholesteatoma at this year’s American Academy of Otolaryngology-Head and Neck Surgery. Information about that presentation can be found here.
Advertisement
Advertisement
Patient with cerebral palsy undergoes life-saving tumor resection
Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.
Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor
Case study illustrates the potential of a dual-subspecialist approach
Evidence-based recommendations for balancing cancer control with quality of life
Study shows no negative impact for individuals with better contralateral ear performance
HNS device offers new solution for those struggling with CPAP
Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition