Ruling out endocarditis is essential when evaluating for systemic vasculitis
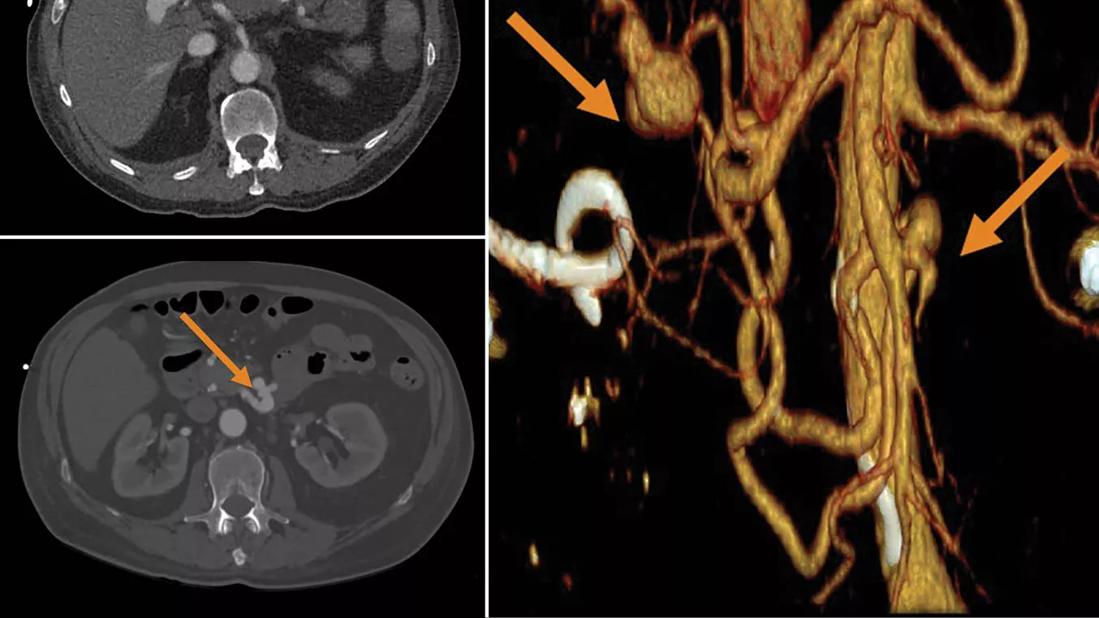
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b300ab32-1029-4b8e-9fea-5c6113e162fe/22-RHE-3091670-yaseen-endocarditis-CQD-jk_jpg)
22-RHE-3091670-yaseen-endocarditis-CQD-jk
Top left: inferior pancreaticoduodenal artery aneurysm. Bottom left: distal right hepatic artery aneurysm. Right: distal right hepatic artery aneurysm and inferior pancreaticoduodenal artery aneurysm.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The vasculitides are a rare group of disorders that cause inflammation of the blood vessel wall (vasculitis) that can lead to vessel destruction, resulting in either stenosis or aneurysm. The differential diagnosis of systemic vasculitides is broad and includes autoimmune disorders such as systemic lupus erythematosus sarcoidosis, various malignancies, and infections such as infective endocarditis and mycobacterial or fungal disease.
Here we report on a patient who was referred for evaluation of possible polyarteritis nodosa (PAN).
A 70-year-old male with a medical history significant for aortic valve replacement presented to Cleveland Clinic for evaluation of acute-onset abdominal pain, high grade fever, chills and unintentional weight loss over a one-month period.
Physical examination on presentation was notable for temperature of 102°F, heart rate of 120 beats per minute, mild abdominal tenderness without guarding or rebound, normal arterial pulses without bruits, and a 3/6 systolic murmur best heard at the right upper sternal border.
Laboratory testing revealed white blood cell count 25k (neutrophils 96%), hemoglobin 8.5 g/dL, elevated sedimentation rate 77 mm/hr, C-reactive protein 17 mg/dL, and normal lipase, kidney and liver function. He tested negative for hepatitis B and C and had a normal hypercoagulable panel. Blood cultures were sent from the emergency department upon admission.
Imaging revealed hemorrhagic cholecystitis on right upper quadrant ultrasound with computed tomography arteriogram showing severe acute pancreatitis, 80% stenosis of the celiac artery at the origin, irregularity of the splenic artery without clear dissection, splenic infarction, a small aneurysm of the inferior pancreaticoduodenal artery, and a 3-cm aneurysm of the distal right hepatic artery.
Transthoracic echocardiogram showed a decreased left ventricular ejection fraction of 40%, moderate-severe aortic insufficiency, thickened mitral valve leaflets and mild mitral regurgitation without vegetations. Later, blood cultures grew Enterococcus faecalis; transesophageal echocardiogram revealed large vegetations on prosthetic aortic valve.
He was diagnosed with endocarditis. Management included embolization of his right hepatic artery aneurysm by interventional radiology, redo aortic valve replacement and intravenous (IV) antibiotics for six weeks.
Advertisement
Infective endocarditis mimicking polyarteritis nodosa endocarditis is a great imitator of the primary systemic vasculitides clinically, radiologically and histopathologically through two mechanisms: embolic phenomena or immune-complex formation.
Due to septic embolization of vegetations to the arterial vasa vasorum, mycotic aneurysms can occur as a rare complication of endocarditis.
The most common causative pathogens are Staphylococcus, Streptococcus and Gram-negative bacilli in IV drug users. Mycotic aneurysms favor arterial branching points and may occur in any vessel; however, the most commonly involved vessels include the aorta and the femoral, cerebral and visceral arteries (renal, hepatic and superior mesenteric artery). Aneurysms due to endocarditis carry a risk of rupture in up to 24% of cases, which is associated with a 66% rate of mortality.
The clinical presentation is varied and consists of localized symptoms depending on aneurysm location and systemic symptoms such as fever, myalgia and weight loss, which are also frequently found in patients with PAN. Patients with endocarditis and mycotic aneurysms may have leukocytosis, anemia, thrombocytosis and elevation of acute-phase reactants similar to PAN. However, in contrast to PAN, endocarditis may cause leukopenia and thrombocytopenia, which are not usually seen in primary systemic vasculitides.
Aneurysms in endocarditis usually manifest as saccular aneurysms with concentric or eccentric periaortic gas and inflammatory soft tissue stranding in 48% of cases, which may help in differentiating from aneurysms related to PAN.
Despite such a distinction, it remains challenging to differentiate both conditions based on radiographic findings only. Notably, these aneurysms typically lack calcification or thrombus as is usually seen in atherosclerosis.
Endocarditis may also mimic anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis by causing constitutional symptoms, cutaneous purpura, digital ischemia, pulmonary cavitary lesions, pauci-immune glomerulonephritis, and positive ANCA testing.
Advertisement
Hence, ruling out endocarditis is essential when evaluating for systemic vasculitis by sending blood cultures and performing transthoracic and/or transesophageal echocardiography.
At Cleveland Clinic’s Center for Vasculitis Care and Research, we work closely as a multidisciplinary team with vascular medicine physicians, cardiologists, cardiovascular surgeons and others in diagnosing and managing challenging vasculitis cases and to rule out vasculitis mimics.
Advertisement
Advertisement
Researching the biological basis for why treatment is or is not effective
Scribing system helps create more face-to-face interactions
A conversation with Leonard Calabrese, DO
The case for continued vigilance, counseling and antivirals
High fevers, diffuse rashes pointed to an unexpected diagnosis
No-cost learning and CME credit are part of this webcast series
Summit broadens understanding of new therapies and disease management
Program empowers users with PsA to take charge of their mental well being