Cardiac magnetic resonance can quantify interaction of size and severity
The use of cardiovascular magnetic resonance imaging (CMR) offers significant prognostic value in assessing patients with ischemic cardiomyopathy (ICM), thanks to its ability to quantify the interaction of ischemic mitral regurgitation (IMR) severity and infarct size. So finds a recent study published in JACC: Cardiovascular Imaging led by Deborah Kwon, MD, Director of CMR in the Section of Cardiovascular Imaging in Cleveland Clinic’s Department of Cardiovascular Medicine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Kwon’s previous research demonstrated that quantifying adverse left ventricular (LV) remodeling and infarct size with CMR improves risk assessment in patients with ICM. “It predicts ischemic MR progression and the success of surgical valve interventions very accurately in these patients,” says Dr. Kwon. “We know that we need to assess remodeling, regurgitation-induced volume changes and infarct size. Our current study is the next step in exploring whether a relationship among those factors can help predict which patients might benefit from therapies or transcatheter-based interventions.”
Dr. Kwon and colleagues performed a retrospective study evaluating 578 patients (mean age, 62 years) with a diagnosis of ICM with LV systolic dysfunction who were referred to Cleveland Clinic for assessment with CMR from 2002 to 2013. CMR was used to quantify infarct size as the proportion of LV mass and to quantify IMR using the mitral regurgitant fraction (MRFraction), an established index of MR severity that accounts for LV stroke volume. The team measured the interaction of CMR-quantified IMR severity and infarct size in relation to a combined endpoint of transplant or death.
Patients had an average LV ejection fraction of 25%, with an MRFraction of 18% and infarct size of 24% of LV mass. Mean follow-up was 4.9 years.
Results showed that, after controlling for several variables, the presence of both large infarct size (≥ 30% of LV mass) and significant IMR (MRFraction ≥ 35%) was strongly associated with all-cause mortality or transplant (P = 0.008) regardless of surgical intervention. Patients with small or moderate infarct size (≤ 29% of LV mass) and significant IMR showed no significant difference in the primary endpoint. Furthermore, patients with smaller infarcts showed a survival benefit with surgical mitral valve intervention.
Advertisement
For patients who are not surgical candidates, transcatheter interventions are a potential alternative. The recent COAPT trial showed significant improvement in survival in patients who received MitraClip®, a percutaneous alternative to open valve surgery, compared with medical therapy. However, MITRA-FR showed no mortality improvement from MitraClip versus medical therapies. Some have hypothesized that COAPT patients had more disproportionate mitral regurgitation (MR degree and LV size mismatch) compared with MITRA-FR patients. The results of the current study provide another dimension to these discussions.
“We showed that ischemic MR severity alone is not enough for accurate prognosis,” says Dr. Kwon. “It must be evaluated in the context of infarct size. Interestingly, left ventricular dilation did not emerge as a significant discriminator of risk or response to surgical intervention in the setting of ischemic mitral regurgitation in our study population. However, infarct size greatly modulated the risk associated with significant ischemic MR. Our findings suggest that quantifying infarct size by CMR might improve patient selection for therapies such as MitraClip.”
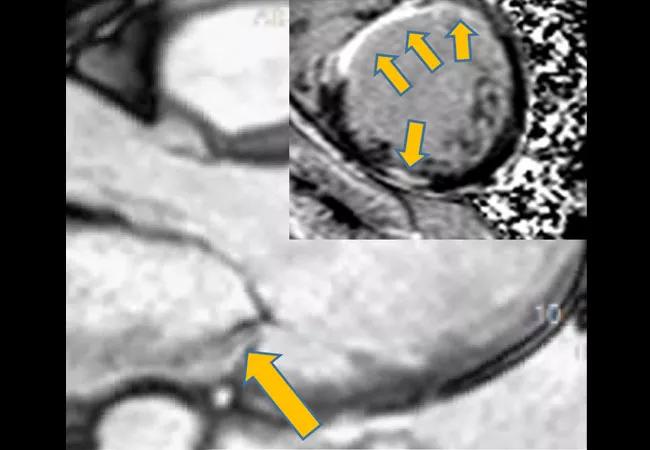
Whether patients with significant IMR (shown in brief video below) and larger infarcts might still benefit from a less-invasive therapy like MitraClip remains to be seen, according to Dr. Kwon. “Our results show a lack of surgical benefit for patients with both large infarcts and high MR fractions,” she says, “but a large, prospective trial is necessary to determine how infarct size impacts outcomes following MitraClip.”
Advertisement
For now, the use of CMR to quantify both infarct size and IMR severity is an important addition to prognostication for patients with ICM.
“Echocardiography alone does not allow the clinician to assess both IMR severity and infarct size,” notes study co-author Brian Griffin, MD, Section Head of Cardiovascular Imaging at Cleveland Clinic. “Combining it with CMR allows for better understanding of the pathophysiology and more-comprehensive risk assessment, which can potentially improve patient selection and procedural outcomes.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more