Retrospective study shows good durability of well-functioning bicuspid valves
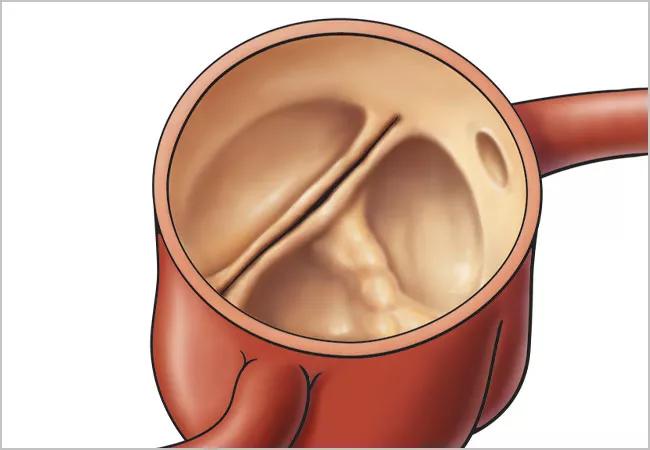
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a3ea4e5e-153d-47c0-9118-7afa26d6abed/22-HVI-3030688_bicuspid-aortic-valve_650x450_jpg)
22-HVI-3030688_bicuspid-aortic-valve_650x450
A well-functioning bicuspid aortic valve (BAV) should be preserved in select patients undergoing isolated ascending aortic replacement, concludes a new retrospective study from Cleveland Clinic. “With this approach, the valve tends to prove durable in the long term, showing slow progression of regurgitation or stenosis and low likelihood of requiring replacement through 10 years,” says cardiothoracic surgeon Eric Roselli, MD, first author of the study, published online in the Journal of Thoracic and Cardiovascular Surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
BAV is a relatively common congenital defect — present in up to 2% of U.S. adults — associated with proximal aortopathy that heightens the risk of aortic dissection or rupture. This risk argues for early intervention in cases of ascending aortic aneurysm, even in the context of a well-functioning valve. However, consensus has been lacking on how best to manage a well-functioning BAV during surgical treatment of an ascending aortic aneurysm — i.e., with preservation or via replacement with either a mechanical valve or a bioprosthetic valve.
“Cleveland Clinic has accumulated a sizeable experience with preservation of well-functioning bicuspid aortic valves in the setting of ascending aortic surgery, so we analyzed this experience with a threefold goal: to characterize aortic and BAV morphology, to evaluate progression to aortic regurgitation or stenosis, and to determine the likelihood of later aortic valve replacement,” explains Dr. Roselli, Cardiac Surgery Director of Cleveland Clinic’s Aorta Center.
The study drew from all 1,872 patients with a BAV who underwent elective primary ascending aortic surgery for dilation, aneurysm or dissection — with or without aortic valve replacement — at Cleveland Clinic from January 1991 to August 2011.
After exclusion of patients who underwent concurrent aortic valve replacement or valve-sparing root reconstruction, as well as patients with moderate to severe aortic stenosis or greater than moderate aortic regurgitation (i.e., a non-well-functioning BAV), the final study cohort consisted of 191 patients with a well-functioning BAV whose primary surgical indication was BAV-associated aortopathy with a presumed ascending phenotype. Mean patient age was 51 years, and 71% of the cohort was male. Seventy-eight of the 191 BAVs were left fully intact, with the remaining 113 undergoing minimal repair based on surgeon judgment.
Advertisement
Outcomes of interest were postoperative aortic regurgitation grade and transvalvular aortic gradient (as assessed by transthoracic echocardiography), reoperation for aortic valve replacement and all-cause mortality. Median follow-up was 10 years.
Morphology. Patients’ mean maximum ascending aortic diameter was 5.1 ± 0.49 cm, and all patients had a cusp-fusion BAV phenotype.
Progression of aortic regurgitation/stenosis. Progression to severe aortic regurgitation over 15 years was 3.2%. The mean aortic valve gradient was 12 mmHg three months postoperatively and started to increase linearly five years after surgery, reaching 27 mmHg by 14 years.
Aortic valve replacement. Freedom from aortic valve replacement was as follows:
The patients who underwent minimal aortic valve repair did not have an increased risk of future aortic valve replacement.
Mortality. Operative mortality was 0%. Survival was as follows:
Only one of the 25 deaths during follow-up was deemed to be valve-related. Operative risk for reoperations in the study was 0%.
“Preserving a well-functioning bicuspid aortic valve in the setting of elective supracoronary ascending aorta surgery is safe,” Dr. Roselli observes. “We found slow progression to severe aortic stenosis or regurgitation, rates of freedom from aortic valve replacement comparable to those with bioprosthetic valves, and long-term survival similar to that of the general population after matching for age, sex and race.”
Advertisement
He notes that while valve durability with valve preservation may not match that of replacement with a mechanical valve, the latter comes with the need for lifelong anticoagulation, which many patients wish to avoid.
He adds that although a direct comparison of the current study population with patients undergoing bioprosthetic aortic valve replacement would be ideal, “our tendency to preserve well-functioning bicuspid aortic valves makes finding a comparable cohort of middle-aged patients who underwent bioprosthetic valve replacement impractical.”
In their study report, the researchers share several implications of their findings for managing patients with a BAV who need isolated ascending aortic replacement:
Another key clinical implication is the centrality of serial echocardiographic monitoring. “We perform routine postoperative echocardiographic follow-up in these patients, even those with a well-functioning bicuspid aortic valve,” says study co-author Milind Desai, MD, MBA, Cardiology Director of Cleveland Clinic’s Aorta Center. “We do so at a minimum of every five years, and more often if there is some evidence of valve dysfunction. We believe this approach helped us avoid the need for any emergency surgeries among patients in our study who ultimately needed aortic valve replacement.”
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon
How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR
Optimal management requires an experienced center