Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve
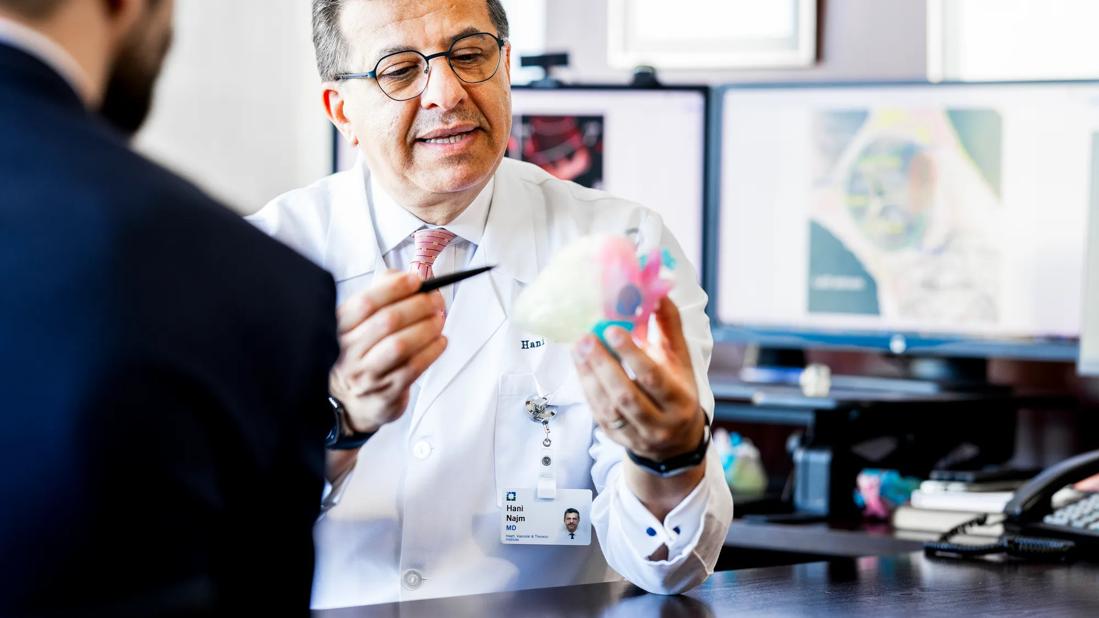
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4ae65792-d244-4d32-a52d-1bc4112fe2a6/CHP_5526166_01-27-25_010_LDJ)
Dr. Najm with colorful 3D-printed heart model
Ventricular switch is a surgical alternative to single-ventricular, Fontan physiology for select patients with complex congenital heart conditions. The novel operation is a combination of more common procedures that essentially switch the functions of the right and left ventricles. Ultimately, blood flows from the left ventricle to the pulmonary artery, and from the right ventricle to the aorta.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“For the past 20 years, many publications have touted the single-ventricular pathway and Fontan physiology as the simplest fix for some patients whose left ventricle cannot be routed to the aorta or adequately support systemic circulation,” says Hani Najm, MD, Chair of Pediatric and Adult Congenital Heart Surgery at Cleveland Clinic. “These patients usually do well for a decade or more. However, they eventually come to us with heart, liver, kidney and other organ failure. We now know that literally every Fontan — where you attach the venae cavae directly to the pulmonary artery, bypassing the heart — will fail at some point. Univentricular repair is not always the best solution for patients. Biventricular repair may be more complex initially, but the outcomes can be better, without inevitable multiorgan failure.”
Dr. Najm, who developed ventricular switch and performed the first procedure in 2016, published outcomes of his first five patients in 2021. Since then, Cleveland Clinic has continued refining the procedure. Now, Dr. Najm and colleagues have published results from a series of 17 patients (Eur J Cardiothorac Surg. 2025 Jul 1;67(7):ezaf155), updating outcomes and sharing what they’ve learned.
Ventricular switch, or right-ventricular-based biventricular conversion, can be used to treat patients with either a hypoplastic left ventricle (but sufficiently sized right ventricle) or anatomy that otherwise prevents systemic circulation from originating in the left ventricle (e.g., malpositioned aorta).
Advertisement
Several surgical techniques may be required to create biventricular circulation. Depending on the patient’s unique anatomy, techniques may include:
All techniques are not required for each patient.
As all ventricular switch procedures are personalized, 3D modeling is important for preoperative planning. MRI or CT is used to construct 3D replicas of each heart, with cardiac structures differentiated by color. The surgical team uses each 3D model to determine whether biventricular conversion is feasible and to define surgical steps in detail.
According to Dr. Najm, advanced imaging and 3D printing enable surgeries like ventricular switch, which once were considered too complex to attempt safely.
“Ventricular switch represents a paradigm shift in congenital surgery, offering a durable biventricular solution that may spare countless patients the progression to Fontan failure and the need for heart-liver transplantation,” says Edward Soltesz, MD, MPH, Surgical Director of Cleveland Clinic’s Kaufman Center for Heart Failure Treatment and Recovery. “The key is early identification of suitable candidates so they can realize the full long-term benefit of this transformative approach.”
In the retrospective study of the first 17 patients (median age 5.2 years, ranging from 4 months to 47 years) treated with ventricular switch at Cleveland Clinic between 2016 and 2023, five (30%) presented with stroke, multiorgan dysfunction or Fontan failure. Most of the patients had a history of complex heterotaxy. They had been selected for ventricular switch because left-ventricle-based biventricular circulation was not feasible.
Advertisement
Immediately after ventricular switch surgery in these patients:
While three (18%) patients had in-hospital mortality — one due to ischemic stroke while on ECMO and two due to preexisting multiorgan failure — none (0%) had 30-day mortality. One-year survival was 79%. Five-year survival was 72%.
During a mean follow-up period of nearly 24 months, five (29%) of the patients had a reintervention, such as percutaneous valve replacement in the conduit or pulmonary artery banding.
One month or more after surgery, echocardiography showed sufficient subpulmonary ventricular function in all 14 patients and sufficient subsystemic ventricular function in 12 patients. All 14 patients had oxygen saturation higher than before surgery, with 12 having saturation greater than 90%.
“Overall, ventricular switch has helped improve cyanosis, oxygen saturation, ventricular function and functional status (or exercise tolerance) in patients who conventionally may have been considered unsuitable for biventricular circulation,” says study coauthor Munir Ahmad, MD, a congenital heart surgeon at Cleveland Clinic. “Our midterm results have been generally favorable in patients with a range of cardiac anomalies, showing the broad utility of this procedure.”
Advertisement
Among the key lessons learned from these patients are:
“The short-term and long-term survival of these patients is dependent on the function of the right ventricle, which becomes the systemic ventricle,” says Dr. Ahmad. “Therefore, it is imperative to thoroughly assess right ventricular function preoperatively.”
Cleveland Clinic now evaluates patients during “switch boards,” gatherings of specialists similar to cancer center tumor boards. Heart surgeons, cardiologists and cardiac imaging specialists review a checklist of criteria for each patient being considered for ventricular switch.
“Switch boards help us assess criteria systematically,” Dr. Najm says. “Because ventricular switch and the congenital conditions addressed are so complex, we must ensure no detail is missed.”
Among the criteria for ideal ventricular switch candidates are:
A full list of considerations is available in the published study.
Sometimes, right ventricular function can fail after ventricular switch because of the tricuspid valve, which normally is not subject to systemic pressures.
“We have started preemptively performing annuloplasty for the tricuspid valve to ensure the valve will not dilate against high pressure and will not fail, causing failure of the ventricle,” Dr. Ahmad says.
Patients with univentricular physiology who present due to Fontan failure and subsequent multiorgan failure tend to have worse outcomes of ventricular switch than do patients who have the surgery sooner, note the surgeons.
Advertisement
“The outcomes are much better when we do ventricular switch before Fontan failure, and even instead of a Fontan procedure,” Dr. Najm says. “We recommend that patients are referred to us as soon as they show any sign of failure, assuming they have a left ventricle that was not previously rerouted. We will make an initial assessment and recommend appropriate candidates for full review by the switch board.”
Heart specialists should consider early conversion of any patient with Fontan physiology and two ventricles to biventricular circulation, he says. Even if left-ventricle-based conversion is selected instead of ventricular switch, do it before the patient has failure.
“I encourage congenital surgeons to learn the techniques for ventricular switch,” Dr. Najm adds. “Individually, the techniques are not complex. It is much better to provide this surgical treatment at the outset rather than as a reoperation later in a patient’s life, after another surgical treatment has failed.”
Advertisement
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
Reproducible technique uses native recipient tissue, avoiding risks of complex baffles
A reliable and reproducible alternative to conventional reimplantation and coronary unroofing
Program will support family-centered congenital heart disease care and staff educational opportunities
Case provides proof of concept, prevents need for future heart transplant
Pre and post-surgical CEEG in infants undergoing congenital heart surgery offers the potential for minimizing long-term neurodevelopmental injury
Science advisory examines challenges, ethical considerations and future directions
Updated guidance and a call to action