New review distills insights and best practices from a high-volume center
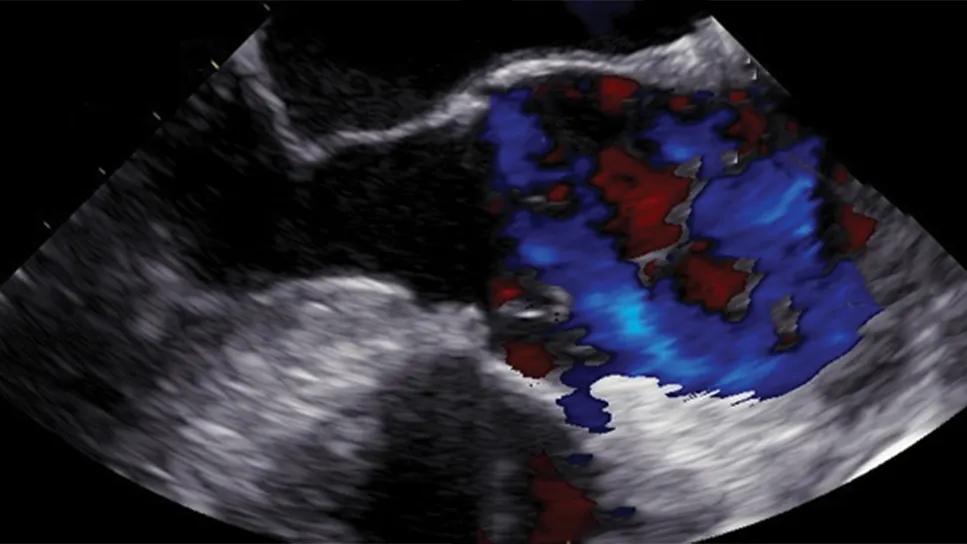
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/403937ff-0a44-413a-8439-24463c81112a/transesophageal-echocardiogram-cqd-feature)
transesophageal echocardiogram showing type A aortic dissection
Acute type A aortic dissection (TAAD) is a challenging cardiac surgical emergency that demands swift and precise intervention to navigate its high mortality risk. While CT angiography serves as the primary diagnostic tool for initial assessment in stable patients, the dynamic nature of TAAD requires real-time imaging during surgery. A recent comprehensive review from Cleveland Clinic cardiac surgeons and anesthesiologists (J Am Soc Echocardiogr.2025;38:498-508) details the critical role of intraoperative transesophageal echocardiography (TEE) in guiding surgical management of acute TAAD and improving patient outcomes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“TEE is far more than a confirmatory diagnostic tool in type A aortic dissection,” says co-author Eric Roselli, MD, Cardiac Surgery Director of the Aorta Center at Cleveland Clinic. “TEE serves as a dynamic, continuous monitor and a strategic guide that adapts to the changing intraoperative landscape. Its ability to provide real-time visualization of the dissection flap, identify new tears, assess cardiac function and distinguish between true and false lumens directly impacts surgical choices, from cannulation strategy to the extent of aortic repair. As a high-volume aorta center, we undertook this review to identify and share insights on intraoperative TEE use that are relevant for guiding and optimizing surgical management of acute type A dissections.”
Although acute TAAD occurs infrequently (4 to 30 cases per million annually), it affects younger populations relative to other cardiovascular emergencies and can be gravely lethal: Mortality rates can surge by 1% to 2% per hour following dissection, usually due to aortic rupture; even for patients who reach the operating room, 30-day mortality ranges from 8% to 40%.
While CT angiography offers high resolution and diagnostic accuracy for initial evaluation, a patient’s aortic condition can change significantly by the time of arrival in the operating suite. TEE meets the resulting need for real-time imaging for surgical guidance, offering continuous assessment and immediate availability, which can be crucial in emergency settings where hemodynamic instability is a concern.
Advertisement
The new review paper leveraged Cleveland Clinic’s institutional experience with intraoperative TEE from patients undergoing surgery for acute TAAD, outlining the modality’s utility throughout the surgical journey, as recapped below.
Diagnosis and extent of dissection. TEE is invaluable for confirming the presence of a dissection flap, identifying any entry tears and mapping the extent of the dissection. Notably, TEE can reveal new tears — especially in the distal arch or proximal descending aorta — that might have developed since initial CT angiography. “Identifying new tears directly influences the surgical strategy, potentially requiring more extensive repairs like full arch replacement or a frozen elephant trunk (FET) procedure,” notes cardiothoracic surgeon Marijan Koprivanac, MD, MS, another co-author of the paper. “TEE also provides uniquely dynamic visualization of the intimal flap throughout the cardiac cycle.”
While TEE has comparable sensitivity and specificity to CT angiography and MRI for detecting dissection flaps, its immediate availability and continuous assessment capability offer distinct advantages. Its chief limitations are the creation of a “blind spot” in the ascending aorta and proximal arch due to anatomical interference, as well the potential for artifacts mimicking dissection flaps.
Hemodynamic monitoring. TEE is critical for recognizing and managing potential hemodynamic decompensation, including the following:
Cardiac tamponade.TEE findings such as hypoechoic effusion around the heart, diastolic collapse of the right ventricle, systolic collapse of the right atrium and inferior vena cava dilation all suggest tamponade. Rapid detection prompts immediate sternotomy and pericardial opening, which can be lifesaving. The authors emphasize that progressive tachycardia with preserved mean arterial pressure can be an early sign of evolving tamponade, requiring traditional “anti-impulse” therapies to be discontinued. Gradual drainage and communication among the surgical team are vital to prevent rebound hypertension and aortic rupture.
Advertisement
Myocardial ischemia.With an incidence of 3% to 5% in acute aortic dissection, myocardial ischemia can be the initial presentation of acute TAAD or develop after initial presentation or during the procedure. TEE helps identify mechanisms such as dissection extension into coronary ostia, intimal detachment, false lumen bulging and dynamic ostium obstruction. TEE reveals dynamic left ventricular wall motion abnormalities or right ventricular dysfunction, prompting careful inspection of the coronary ostia.
Aortic valve assessment. TEE allows for precise assessment of the severity and mechanism of aortic insufficiency, guiding decisions between aortic valve repair and replacement. TEE findings that support consideration of valve repair include the absence of intrinsic valve disease, aortic insufficiency caused by flap intussusception, and dilation of the annulus, root or ascending aorta. Direct surgical inspection is always necessary to confirm the feasibility of repair.
Assessment of branch vessel flow. While the aortic arch vessels are typically TEE blind spots, TEE can be helpful for assessing patency of the celiac trunk and, to a lesser extent, the superior mesenteric artery. It also helps determine whether branch vessels originate from the true or false lumen, whether dissection extends into the vessel and whether the flap is causing dynamic obstruction of the branch vessel origin. Analyzing color-flow Doppler characteristics can be useful for timely identification of patients at risk for mesenteric ischemia.
Advertisement
True lumen identification and cannulation guidance. TEE plays a pivotal role in guiding direct central aortic cannulation — i.e., at a site where the cannula can be dynamically repositioned. The review highlights that many previously described characteristics for differentiating true and false lumens in the descending aorta (e.g., color dominance, velocity, flap movement, lumen size, thrombus/cobwebs) are often unreliable or rare. The most reliable TEE finding for distinguishing true from false lumens in the descending aorta is a clear, circumferential intimal delineation of the true lumen, accompanied by a crescent appearance of the false lumen on short-axis views. If this reliable differentiation is not possible, it must be communicated to the surgeon, potentially requiring revision of the cannulation strategy or surgical plan, such as opting for an FET procedure.
Perfusion confirmation. After cardiopulmonary bypass is started, TEE is essential for confirming true lumen perfusion regardless of the cannulation strategy. It can help detect malperfusion caused by issues like cannula abutment against the intimal layer or a 360-degree circumferential flap that adheres to the cannula, potentially compromising proximal flow (e.g., to the brain). In such cases, TEE guides repositioning of the cannula until optimal flow is restored.
Ongoing monitoring. TEE assessment should be performed periodically: after aortic cross-clamping, right after resuming circulation following circulatory arrest (especially with FET procedures to confirm stent graft position in the true lumen) and after separating from bypass to reconfirm stent graft position and distal patency.
Advertisement
Guiding extent of surgery. Real-time TEE findings can inform decisions about the extent of surgical repair. For instance, a severely compressed true lumen in the descending aorta or an unidentified arch tear seen on TEE might prompt the surgeon to consider a more extensive repair like FET or specific arch repair zones, even if not initially indicated by static CT angiography.
Prognostic evaluation. Thorough TEE evaluation of the aorta after cardiopulmonary bypass remains crucial for early identification of any persistent false lumen patency, guiding potential further interventions to prevent postoperative malperfusion complications.
“Our Cleveland Clinic experience, as distilled in this review, reveals TEE to be a cornerstone of the surgical management of acute TAAD,” Dr. Roselli says. “TEE is also proving to be a critical tool as we continue to develop endovascular therapies for the higher-risk subset of patients with acute dissection, such as in the ARISE clinical trials.”
“The utility of TEE spans the surgical process,” Dr. Koprivanac adds. “It ranges from confirming diagnosis and assessing the comprehensive status of the aorta and its branch vessels before bypass to guiding precise cannulation, monitoring perfusion and assessing repair results post-bypass. In a condition where every minute counts and intraoperative findings can change dramatically, TEE provides the dynamic, real-time insights needed to make lifesaving surgical decisions.”
“TEE’s role in patients presenting with acute type A dissection has significantly broadened from use for initial diagnosis when CT angiography is contraindicated to an extremely important intraoperative procedural imaging guide,” observes Vidyasagar Kalahasti, MD, a staff cardiologist with Cleveland Clinic’s Aorta Center. “Intraoperative TEE is useful not only to identify true and false lumen but also to assess left ventricular and aortic valve function in real time, helping with surgical strategy and immediate postsurgical care.”
Advertisement
New Cleveland Clinic data challenge traditional size thresholds for surgical intervention
Study finds comparable midterm safety outcomes, suggesting anatomy and surgeon preference should drive choice
Blood test can identify patients who need more frequent monitoring or earlier surgery to prevent dissection or rupture
Recent Cleveland Clinic experience reveals hundreds of cases with anatomic constraints to FEVAR
Multicenter pivotal study may lead to first endovascular treatment for the ascending aorta
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Large cohort study finds significant effect in men and nonsmokers
Impacts include major emphases on multidisciplinary teams, shared decision-making