Study finds comparable midterm safety outcomes, suggesting anatomy and surgeon preference should drive choice
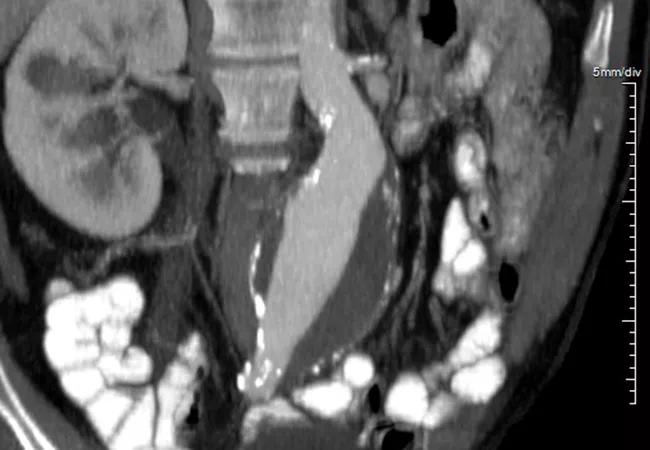
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/66bd081e-39a2-4c9e-8524-258c4ae07290/21-HVI-2595510_aortic-aneurysm_650x450-jpg)
imaging scan of abdominal organs
Both transperitoneal (TP) and retroperitoneal (RP) approaches to abdominal aortic aneurysm (AAA) repair are safe in women, so patient anatomy and surgeon preference should drive decision-making about choice of technique in female patients. So concludes a retrospective midterm outcomes study by Cleveland Clinic researchers published in Vascular (2025;33[3]:511-519).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Mortality in women with AAA is high, yet there has been little evidence to date to guide selection of surgical approach in female patients. “To our knowledge, this is the first study to compare transperitoneal and retroperitoneal open aortic aneurysm repair in a female population,” says senior author Francis Caputo, MD, Vascular Surgery Director of Cleveland Clinic’s Aorta Center. “Over the 12-year period studied, results of these surgeries in women were similar on midterm analysis, showing minimal complications in experienced hands.”
The prevalence of AAA is higher in men than in women, yet women with the condition are more likely to die or have serious complications. Rapid AAA expansion is more common in women, who also have quadruple the risk of rupture at a small diameter. Even when repair is possible, rates of postsurgical complications, morbidity and mortality are elevated in women, possibly because of older age at diagnosis or anatomic issues.
Results of studies comparing open AAA repair outcomes with RP and TP approaches have been mixed, and none have looked specifically at outcomes in women. The Cleveland Clinic study aimed to address that gap by comparing outcomes and complications specifically in a female population in both elective and emergency settings.
Study data came from 244 female patients who underwent open AAA repair using an RP or TP approach from 2010 to 2021. The RP and TP cohorts were comparable in patient age (mean of 70.8 ± 9.3 years overall) and in perioperative characteristics, with two exceptions: elevated ejection fraction (>50%) was more common in the RP group, and American Society of Anesthesiologists (ASA) class was significantly higher in the TP group, indicating worse physiologic status.
Advertisement
Outcomes including mortality and graft- and non–graft-related complications were analyzed over mean follow-up of 28 ± 30.7 months. Multivariable analysis was performed with adjustment for age, urgency, smoking, prior aneurysm repair and ASA class.
Of the 244 patients, 133 underwent the RP approach and 111 the TP approach. Across the overall cohort, 81.7% of patients received elective repair, 10.1% underwent repair for AAA rupture and 7.5% underwent symptomatic repair. Distribution of surgical urgency was similar between the RP and TP groups.
Compared with TP repair, the RP approach was associated with significantly longer visceral/renal ischemia time, larger graft diameter (18 vs. 16 mm; P < .001), increased likelihood of suprarenal clamp placement and lower autotransfusion volume.
More patients in the TP group died during follow-up (P = .035), but the difference in time-to-event analysis was insignificant. At 36 months, all-cause survival did not differ between the RP and TP groups.
The overall rate of midterm complications was 9.5% in both groups. The incidence of any graft-related complication was 3% in the RP group versus 1.8% in the TP group (P = .69).
On multivariable analysis, the hazard ratio for mortality was lower in the RP group than in the TP group, but the difference did not reach statistical significance (P = .052). A subanalysis excluding ruptures and aortic repair that required supraceliac clamps also found no significant differences.
“We found that the retroperitoneal approach was more likely to be used for more proximal aneurysm configuration when suprarenal or supravisceral clamping was anticipated,” notes co-investigator Ali Khalifeh, MD, a Cleveland Clinic vascular surgeon. “A bifurcated graft with anastomoses to the common iliac artery or external iliac artery was more likely with the transperitoneal approach.”
Advertisement
The researchers acknowledge that long-term complications may have been underreported in the study cohort because Cleveland Clinic is a quaternary referral center. They also note that they did not account for selection bias for the surgical approach in their analysis.
“Overall, both the retroperitoneal and transperitoneal approaches demonstrated minimal complications, confirming their safety when performed by experienced teams,” Dr. Caputo concludes. “Surgeon expertise and patient-specific considerations are key in selecting the approach to AAA repair, and further research is needed to identify factors that impact outcomes in women.”
Advertisement
Advertisement
New Cleveland Clinic data challenge traditional size thresholds for surgical intervention
New review distills insights and best practices from a high-volume center
Blood test can identify patients who need more frequent monitoring or earlier surgery to prevent dissection or rupture
Recent Cleveland Clinic experience reveals hundreds of cases with anatomic constraints to FEVAR
Multicenter pivotal study may lead to first endovascular treatment for the ascending aorta
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Large cohort study finds significant effect in men and nonsmokers
Impacts include major emphases on multidisciplinary teams, shared decision-making