Study identifies imaging parameters for predicting mortality risk
Isolated tricuspid regurgitation is a high-risk condition and increasingly seen, but its management is controversial. Now a Cleveland Clinic study has demonstrated that adding cardiac magnetic resonance imaging (CMR) to echocardiography and clinical history assessment can help identify which patients have severe valve regurgitation and are most likely to have a poor outcome, with the aim of potentially guiding management decisions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“There are no proven medical therapies that reduce deaths in tricuspid regurgitation,” says the study’s first author, Tom Kai Ming Wang, MBChB, MD, a cardiologist in Cleveland Clinic’s Section of Cardiovascular Imaging. “And unlike the surgical treatment of aortic or mitral valve regurgitation, which has a low in-hospital mortality rate of 2% to 3% nationally and < 1% at Cleveland Clinic, in-hospital mortality rates following surgery for isolated tricuspid regurgitation approach 9% to 10% nationwide. We sought to determine the clinical and multimodality imaging parameters predictive of mortality in these patients in order to define who has severe tricuspid regurgitation and assist in decision-making around surgery and medical management.”
The cohort study was published online in Circulation: Cardiovascular Imaging.
Dr. Wang notes that the poor outcomes associated with isolated severe tricuspid regurgitation may be related to the fact that the condition often doesn’t cause many symptoms. “By the time patients present for evaluation,” he says, “heart remodeling and dysfunction have usually already occurred and are coupled with high lung pressures in patients who often have many other comorbidities, such as heart failure, atrial fibrillation, hypertension and prior cardiac surgery.”
Additionally, studies of multimodality imaging in this setting have been limited. Guidelines for determining tricuspid disease severity are based on transthoracic echocardiography (TTE), Dr. Wang notes. While CMR has been shown to be valuable for evaluating tricuspid regurgitation, its thresholds for severe tricuspid regurgitation are unknown, and the prognostic utility of both imaging techniques together had not previously been studied in this context.
Advertisement
“Although TTE is widely available as the first-line modality to assess the right heart or the tricuspid valve, it has important limitations in these indications,” Dr. Wang explains. “It allows for reasonable qualitative interpretations — such as mild, moderate or severe — but it doesn’t really provide accurate quantitative measurements. We believed that CMR would be useful because it quantifies how much volume of blood is regurgitating through the tricuspid valve with every heartbeat, and it puts a number on it (see figure). It also is the reference standard for right heart measurements that are directly affected by tricuspid regurgitation.”
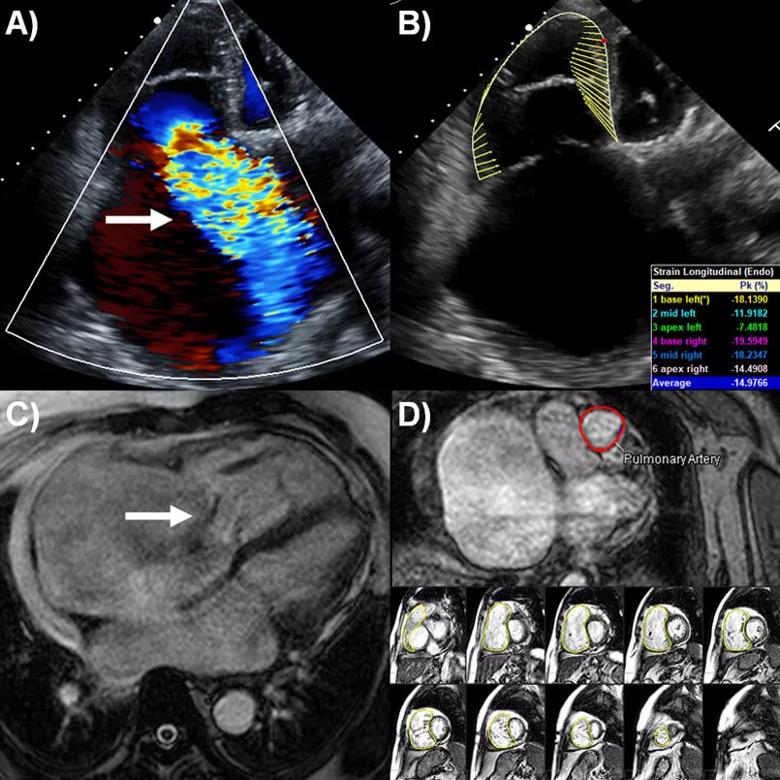
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f77c3c6d-4369-4a6f-8302-8a6dbca4219d/21-HVI-2288858-Inset-805x805-1_jpg)
Figure. Multimodality imaging evaluation of isolated tricuspid regurgitation. (A) Color Doppler of severe tricuspid regurgitation (arrow) in apical right ventricle view by transthoracic echocardiography (TTE). (B) Right ventricular longitudinal strain evaluation by TTE using velocity-vector imaging software (yellow trace). (C) Cine sequence four-chamber view showing severe tricuspid regurgitation (arrow) by cardiac magnetic resonance imaging (CMR). (D) Quantification of tricuspid regurgitation volume (TRRV) and fraction (TRRF) by CMR involving calculation of pulmonary artery forward flow (PA flow; top, red trace) with phase contrast sequence and calculation of right ventricular stroke volume (RVSV; bottom, yellow traces) with cine short-axis stack sequence. TRRV = RVSV – PAflow; TRRF (%) = TRRV/RVSV.
For their study, the researchers identified 262 consecutive patients with at least moderate-to-severe isolated tricuspid regurgitation who underwent CMR (in addition to TTE) at Cleveland Clinic between January 2007 and June 2019. Mean patient age was 62.8 years; 59.5% of the cohort was female; and tricuspid regurgitation etiology was secondary in 79% and primary in 21%.
Advertisement
The study’s primary endpoint was time to all-cause mortality. The researchers mined imaging and clinical data to determine the threshold for severe tricuspid regurgitation by CMR, and multivariable analysis was used to determine factors predictive of mortality.
Over mean follow-up of 2.5 years, 68 patients (26%) died. Survival rates were 84.1% at one year, 69.1% at three years and 61.8% at five years. Among the 87 patients in the cohort (33.2%) who underwent tricuspid valve surgery (70 repairs and 17 replacements), there were five in-hospital deaths. The study’s secondary endpoint — a composite of all-cause mortality and heart failure hospitalization — occurred in 107 patients (40.8%).
On multivariable analysis, the three most important imaging and clinical parameters found to independently predict mortality were:
Additionally, undergoing tricuspid valve surgery was found to be protective against mortality with borderline statistical significance (P = 0.049). This finding was interesting, Dr. Wang notes, as surgery remains controversial in isolated tricuspid regurgitation and some recent studies found no survival benefit from surgery. “Outcomes of isolated tricuspid surgery at other centers are generally quite poor, but the in-hospital mortality rate at Cleveland Clinic was 5.7% in this study and overall is approximately 3%,” he says. “This is related to our surgical expertise and more aggressive approach to performing surgery earlier. The borderline significance in this study may stem from the relatively small sample size of patients undergoing both CMR and surgery.”
Advertisement
“This study indicates that greater tricuspid regurgitation quantification by CMR and lower magnitude of right ventricular free wall longitudinal strain by TTE added incremental prognostic value over conventional risk models in the setting of isolated tricuspid regurgitation,” says the study’s senior and corresponding author, Milind Desai, MD, MBA, Director of Operations in Cleveland Clinic’s Department of Cardiovascular Medicine. “It suggests that combining this multimodality imaging approach with clinical evaluation is a compelling strategy for assessing risk and timing management in this challenging patient population.”
“CMR utilization in isolated tricuspid regurgitation has grown in recent years at Cleveland Clinic, and this study for the first time defines the thresholds for severe tricuspid regurgitation and confirms prognostic utility,” notes Dr. Wang. “Further external validation of the thresholds and risk model we identified is necessary before they are broadly applied clinically to contribute to surgical decision-making.”
He adds that additional investigation is needed on how the newer, less-invasive transcatheter tricuspid valve procedures compare with surgical treatment, including in randomized trials, “and whether our findings can help select patients for those interventions as well, to try and improve outcomes in this condition with otherwise poor prognosis.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more