The case for personalized brain mapping in complex disorders
By Andre Machado, MD, PhD; Imad Najm, MD; and Robert Fox, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Neurological and neurosurgical care in 2018 has expanded dramatically beyond the neurological examination and core operative procedures that formed the bedrock of practice in our disciplines. As contemporary care evolves, the importance of data that is highly personalized for each individual patient with a neurological condition becomes ever more apparent.
This increasing personalization of care has emerged just as the value of multidisciplinary collaboration has grown more and more evident. At Cleveland Clinic, we recognized this development over a decade ago by embracing an institute-based organizational structure. For individuals with brain and spine conditions, this structure brings together neurologists, neurosurgeons, neuroradiologists and neuroscientists in a Neurological Institute organized around patients’ disease-specific diagnostic and management needs rather than traditional departmental groupings. As a result, patients benefit from deeper collaboration across our institute’s 14 subspecialty centers.
One area in which these two trends — increasing personalization and multidisciplinary collaboration — intersect with particular power is in what we describe as “information-guided care.” This concept represents a redefinition of neuroscience care that promotes cross-disciplinary collaboration in pursuit of more-personalized diagnosis and less-invasive management of the most challenging cases of various neurological diseases.
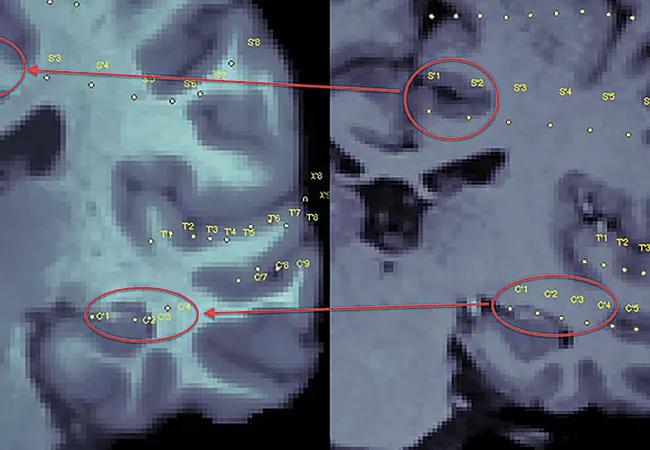
Our multidisciplinary teams in the Neurological Institute are at the forefront of this redefinition, which arises from the use of leading-edge imaging technologies, such as state-of-the-art 7T MRI, in innovative ways and combinations. The objective is threefold: (1) to better visualize brain anatomy, (2) to enhance understanding of function and (3) to provide accurate, noninvasive diagnosis of brain pathology without need for tissue biopsy.
Advertisement
Our multidisciplinary Neurological Institute teams recently published here on Consult QD progress reports from various fronts in their pursuit of personalized, information-guided neurological care. We urge you to check out these brief, image-rich reports for a more detailed take on the fascinating work underway. These reports fall into three broad categories.
First is a series of profiles of how our teams have been untangling the complex connectivities of the brain to create anatomo-functional maps to help tailor personalized treatment options. The specific work covered includes:
Next comes a trio of reports on how we are using novel analytic methods and machine learning to make the most of MRI by enhancing the processing of otherwise routine imaging data. These approaches — which include computer-assisted morphometric assessment of MRI findings, integration of machine learning with MRI post-processing, and quantitative MRI volumetric analysis — promise more straightforward diagnosis across various neurological conditions, without the need for more-complex and invasive diagnostic methods.
Advertisement
We round out our reports with two short articles reviewing our work on clinical application of a novel PET radiotracer that preferentially binds to molecular components of myelin and provides quantitative imaging of brain white matter integrity beyond what’s possible with existing MRI methods. The first article explains the technology, called myelin PET, and how it adds a new dimension to brain mapping. The second article profiles how we have started to use myelin PET to improve lesion identification in pharmacoresistant epilepsy, with studies in multiple sclerosis, stroke rehabilitation and other conditions planned.
We believe this information-guided approach to neuroscience care designed and validated by expert multidisciplinary teams will lead to enhanced diagnosis, more-personalized treatment options and improved outcomes for patients with the most complex neurological diseases.
Dr. Machado is Chairman of Cleveland Clinic Neurological Institute. Dr. Najm is Neurological Institute Vice Chairman for Strategy and Development. Dr. Fox is Neurological Institute Vice Chairman for Research.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help