What to do when a patient’s ischemia is not due to coronary artery stenosis
Ischemia with non-obstructive coronary arteries (INOCA) is an increasingly recognized entity involving microvasculature dysfunction and/or vasospasm of the coronary arteries. Because the diagnosis requires specialized expertise and testing, it is frequently missed. But leaving it undiagnosed puts the patient in peril, as INOCA is associated with repeated emergency department visits and hospital admissions, as well as increased incidence of cardiovascular events and death.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These characteristics have made INOCA an area of great interest for Cleveland Clinic interventional cardiologists Khaled Ziada, MD, and Claire Raphael, MD, PhD.
“Despite poor awareness of INOCA, we now know it is not rare, and that makes it an important topic,” says Dr. Ziada. “Fortunately, we are gaining a better understanding of its mechanisms and how to diagnose and manage it.”
Studies show that more than 50% of patients undergoing invasive angiography — particularly women — do not have obstructive coronary artery disease, with many of them having INOCA.
“I’ve seen many patients who are so grateful for a diagnosis of INOCA after having had their angina symptoms repeatedly dismissed by doctors,” says Dr. Raphael. “Just knowing that their condition is a real entity is a tremendous relief and allows patients to move forward with management.”
Like angina caused by stenosis of the larger coronary arteries, INOCA involves a supply-demand mismatch of myocardial oxygen. Two major mechanisms — microvascular dysfunction and vasospastic disorders — have been identified, as detailed below and illustrated in the figure.
Microvascular dysfunction involves small vessels that supply the myocardium but cannot be seen angiographically. The pathophysiology may be related to vasomotor dysregulation and structural remodeling of the arterioles.
So-called microvascular angina (MVA) is more common in women, especially during middle age. Risk factors are similar to those for atherosclerosis and include smoking, hypertension and dyslipidemia.
Advertisement
PET and MRI criteria have been established for the diagnosis of MVA, but they are not always reliable. Better diagnostic measurements can be performed in the catheterization laboratory: reduced coronary flow reserve and reduced blood flow velocities (using index of microvascular resistance testing) are indicative of MVA and predictive of elevated risk of cardiovascular events and death.
Vasospastic disorders involve spasm of coronary arteries. Hyperreactive smooth muscle cells and dysfunctional endothelium are likely underlying mechanisms. Vasospasm can be transient (causing Prinzmetal angina) or persistent, leading to myocardial infarction.
Vasospastic angina (VSA) more commonly occurs in Asians and men, with smoking being a major risk factor. It can be diagnosed in the catheterization lab, with provocative testing using intracoronary acetylcholine and/or IV ergonovine.
These two INOCA endotypes — MVA and VSA — may overlap, which is associated with a worse prognosis.
“The key is to think about INOCA when we see patients who present with angina but have little or no evidence of plaque in their coronary arteries,” says Dr. Ziada. “Appropriate testing can be done at the same time that we perform angiography.”
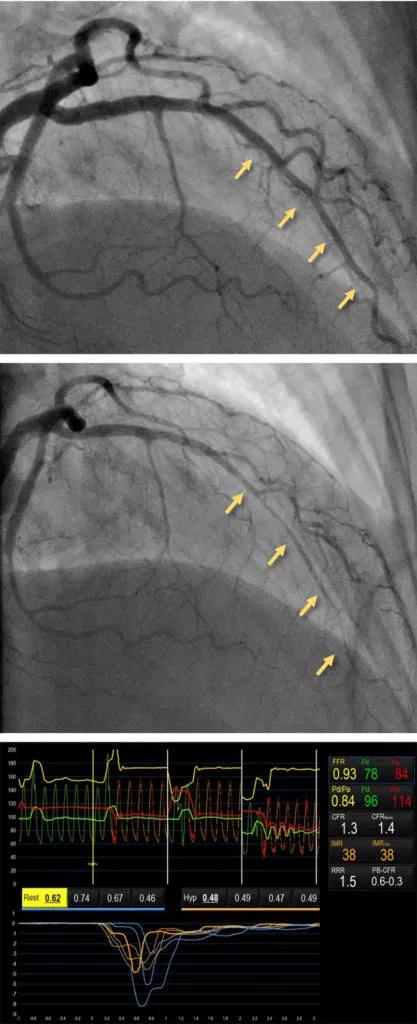
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8f1e059e-a3c4-4614-ae0f-ff9bf504355b/22-HVI-2623150-CQD-inset-417x1024_jpg)
Figure. Acetylcholine provocation testing for coronary spasm and microvascular function testing. Top and middle panels demonstrate angiography of the left coronary system before and after intracoronary injection of acetylcholine 50 micrograms. Severe spasm is noted in the mid and distal left anterior descending artery (arrows) in response to the drug. When accompanied by ECG changes and reproduction of the patient’s chest pain, this is diagnostic of vasospastic angina. The bottom panel demonstrates microvascular function testing in a different patient with INOCA. In this case, coronary flow reserve (CFR) calculated using the thermodilution method is abnormal at 1.3 (normal, >2.0 or 2.5). The index of microcirculatory resistance (IMR) is also abnormal at 38 (normal, <25).
Patients with INOCA need therapy to alleviate their angina symptoms and to address long-term risk of cardiac events. Neither MVA nor VSA can be treated with stents or bypass. Dr. Ziada offers the following guidance on various aspects of management:
Advertisement
Dr. Raphael notes that research is underway on many aspects of INOCA diagnosis and treatment. The large WARRIOR trial (Women’s Ischemia Trial to Reduce Events in Nonobstructive Coronary Artery Disease) is enrolling more than 4,000 patients at multiple sites to assess the impact of intensive medical treatment (high-dose statin, moderate-dose ACE inhibitor, angiotensin II receptor blocker) on death, myocardial infarction, stroke and hospitalization. Participants will be followed for three years, with results expected in 2024.
She is particularly excited about two promising avenues of innovative treatment:
Advertisement
“Our understanding of INOCA is growing quickly, as is physician awareness,” Dr. Raphael observes. “I am hopeful that it will soon be a well-recognized condition with effective therapy options.”
Advertisement
Advertisement

Scenarios where experience-based management nuance can matter most

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients