First reported case expands use of minimally invasive techniques
By Mark Bain, MD, MS; Jianning Shao, BA; and Pablo Recinos, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 50-year-old woman with no significant past medical history was transferred to our center emergently with a diagnosis of acute left intracerebral hemorrhage (ICH), noted severe right-sided hemiplegia and aphasia and a National Institutes of Health Stroke Scale score of 27.
Head CT showed a 6.3-cm hematoma in the putamen of the left basal ganglia (Figure 1).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/160ec561-8d16-44e7-8a31-a40d1989d86e/Preop-basal-ganglia-hemorrhage_png)
Figure 1. Axial head CT revealing 56-cc left basal ganglia hemorrhage.
Reprinted with permission from Shao J, Witek A, Borghei-Razavi H, Bain M, Recinos PF. Endoscopic evacuation of intracerebral hematoma utilizing a side-cutting aspiration device. Oper Neurosurg (Hagerstown). 2019 Oct 12 [Epub ahead of print]. ©2019 by the Congress of Neurological Surgeons.
We obtained a CT angiogram (CTA) to rule out vascular lesions as part of our standard preoperative workup at Cleveland Clinic. Though spot sign was not present, CTA revealed a slight expansion of the parenchymal hematoma and intraventricular extension. The team also noted blood in the ipsilateral ventricle.
Given the hematoma’s size, expansion and presence with intraventricular hematoma (IVH), we explored surgical evacuation, opting for an endoscopic, transcortical approach with a side-cutting aspiration device. Using neuronavigation, we inserted a 19-French peel-away sheath with a 15-gauge side-cutting aspiration device handpiece through a 13-mm burr hole with duratomy and a trans-sulcal approach to access the hematoma. We first addressed the clot in the middle, as it was furthest from eloquent areas. We used the aspiration-only setting of the device to move clot away from parenchymal walls, and then used side-cutting aspiration to diminish the hematoma’s size. Next we began continuous irrigation through the endoscope to expand the cavity for better visualization and mobilization of further clot. We used hemostatic agents and continuous irrigation to achieve endoscopic hemostasis during the procedure. The 13-second intraoperative video below shows aspiration and breaking up of a clot during the case.
Advertisement
An immediate postoperative CT demonstrated clear midline recovery with no evidence of mass effect. The patient began physical therapy on postoperative day 2. When she was discharged on postoperative day 10, she was alert, oriented and slowly regaining strength.
At one-month follow up, axial head CT showed complete resolution of brain shift and little evidence of the surgical tract (Figure 2). The patient was ambulatory but experiencing residual expressive aphasia and right-sided weakness. She continues to improve with appropriate therapies.
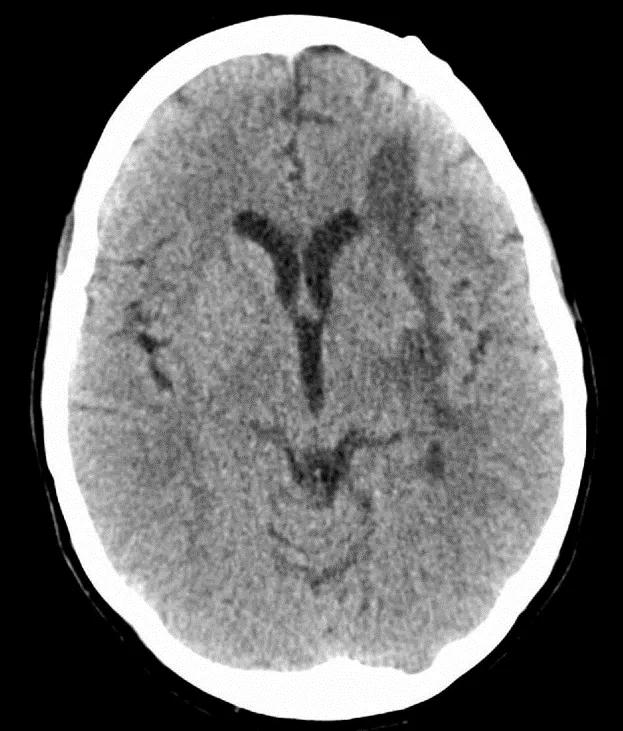
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a4d94ed0-93fb-4eb9-a551-fe4de6aca3a5/Postop-CT_png)
Figure 2. One-month postoperative axial head CT showing complete resolution of brain shift and little evidence of surgical tract. Reprinted with permission from Shao J, Witek A, Borghei-Razavi H, Bain M, Recinos PF. Endoscopic evacuation of intracerebral hematoma utilizing a side-cutting aspiration device. Oper Neurosurg (Hagerstown). 2019 Oct 12 [Epub ahead of print]. ©2019 by the Congress of Neurological Surgeons.
Traditionally, ICH was considered a monophasic disease with little demonstrated benefit from support care or craniotomy and with medical management as the standard of care. More recently, we’ve come to understand ICH as a biphasic disease, with the second phase of injury from perihematomal inflammation and edema accounting for the delayed neurological deterioration we often see in ICH patients. In this model of the disease, time and volume control are critical.
While trials have shown no benefit from craniotomy, the recent MISTIE III trial found a mortality benefit to ICH removal via minimally invasive surgery (MIS), with other studies corroborating the results. A higher degree of hematoma evacuation correlated with improved outcomes in MISTIE III. In contrast to the days-long procedure in MISTIE, our novel technique in this case achieved immediate near-total evacuation, thus reducing mass effect and secondary injury. When time and volume are of the essence, our technique offers a faster, more complete evacuation.
Advertisement
The device we used is one of many new developments in MIS for ICH evacuation. This side-cutting aspiration device features dual functionalities that permit homogenization and removal of clots, while a blunt end reduces parenchymal injury risk. The surgeon modulates suction strength with a foot pedal. Two ongoing studies — Early Minimally Invasive Removal of Intracerebral Hemorrhage (ENRICH) and Prospective, Multicenter Study of Artemis, a Minimally Invasive Neuro Evacuation Device (MIND) — are exploring other MIS devices and early intervention techniques.
Because our patient’s hematoma was stable, her case offered an ideal scenario for side cutting with an endoscopic approach. We recommend early and immediate evacuation, with a preoperative CTA to assess for the presence of arteriovenous malformations or aneurysms. This imaging is part of our standard of care at Cleveland Clinic and is a required part of many clinical trials in this arena. Our operative setup included monitors showing navigation and endoscopic views side by side to optimize visualization. We also had previous experience in the use of this device for evacuation of intraventricular empyema in four patients. Our full report of this ICH case in Operative Neurosurgery provides additional images and video of the surgical technique.
Our experience in this case offers a modification to the stereotactic intracerebral hemorrhage underwater blood aspiration (SCUBA) technique: the first documented use of a side-cutting aspiration device via an endoscopic transcortical approach for evacuation of ICH. While more study is needed, we hope our experience with this patient contributes to efforts to develop a standardized endoscopic approach to treatment of ICH.
Advertisement
Dr. Bain is Head of Cerebrovascular and Endovascular Neurosurgery in Cleveland Clinic’s Cerebrovascular Center. Ms. Shao is a medical student at Cleveland Clinic Lerner College of Medicine. Dr. Recinos is a neurosurgeon at Cleveland Clinic with specialty expertise in skull base surgery.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help