For kids with painful, growing lesions in the arm, leg or pelvis

Pediatric patients with newly identified musculoskeletal lesions can get faster, expert triage and treatment at Cleveland Clinic’s new Pediatric Musculoskeletal Tumor Clinic. The clinic is opening this fall at Cleveland Clinic Children’s, where it will be staffed by pediatric orthopaedic oncology and medical oncology specialists.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The vast majority of lumps and bumps in children are benign,” says pediatric orthopaedic oncologist Zachary D. Burke, MD. “That’s why a big part of our clinic will be reassuring kids and their families that a lesion is not cancer. If it is cancer, our aim is to avoid delayed or missed diagnoses that can happen with this rare disease, and reassure families that they’re in the right place for advanced care.”
The clinic will accept referrals from pediatric, family practice, emergency department (ED), general orthopaedic, sports medicine and other providers.
“We are so excited to put our ‘patients first’ philosophy into action,” says Rabi Hanna, MD, Chair of Hematology and Medical Oncology at Cleveland Clinic Children’s. “The lumps and bumps clinic will bring together a multidisciplinary team of experts and ensure early and coordinated access to outstanding care for all kids and young adults with suspicious musculoskeletal lesions.”
Although Cleveland Clinic already treats pediatric patients with musculoskeletal tumors, patients often take a circuitous route to the appropriate provider.
“Often patients first go to their local ED or pediatrician,” Dr. Burke explains. “They may be advised to watch and wait awhile. Then they may get referred to an orthopaedic surgeon who may not specialize in tumors. Eventually they get referred to a musculoskeletal oncology specialist. All of these extra steps may lead to delayed treatment, incorrect information and, in the worst case, incorrect treatment. By establishing a Pediatric Musculoskeletal Tumor Clinic, we essentially create an open door for ED or primary care providers to send patients with concerning lesions directly to us.”
Advertisement
In addition to saving time, the new clinic will help prevent misdiagnosis of musculoskeletal tumors.
“We’ve seen so many patients who believed they had cancer when they actually didn’t,” Dr. Burke says. “Or, more often, patients tell us that other doctors don’t know what the tumor is. Both of those scenarios can cause stress for patients and their families. Even worse are those who are advised to watch and wait — or receive incorrect treatment — when they actually have sarcoma.”
Getting a prompt, accurate diagnosis is important for all types of tumors, whether benign, benign aggressive or cancerous, he adds. Then appropriate monitoring and treatment can begin right away.
Providers should refer to the clinic any pediatric patient with a lump, bump or lesion that is concerning, specifically one that is:
“Even if imaging looks benign, providers should consider referring lesions that meet the criteria,” Dr. Burke says. “Kids get bruises and sports injuries all the time, and these lesions are often found incidentally. However, lumps that are getting smaller are typically not concerning and do not require referral.”
The clinic is specifically for musculoskeletal lesions, not for lesions in or on the:
Advertisement
“Referral before intervention is critical,” Dr. Burke says. “One of our primary goals is to prevent surgeries or biopsies that can be harmful to patients.”
He emphasizes that if sarcoma is on the differential, any biopsy or intervention should be guided or performed by providers who are experienced in treating sarcoma. Management becomes more challenging and outcomes tend to be worse when operating on tumors that unexpectedly turn out to be sarcoma.
“We want to prevent those situations,” he says. “If there’s any uncertainty about diagnosis of a musculoskeletal tumor, get us involved. We are always happy to help.”
Advertisement
Advertisement

Dedicated investigators and clinicians bring expertise in drug development and flexible study design

Personalized reconstruction is an alternative to leg amputation or flail limb

Soft tissue pathologist discusses research into incorporating genomic data to improve risk stratification

Machine learning models assess intraoperative tissue perfusion
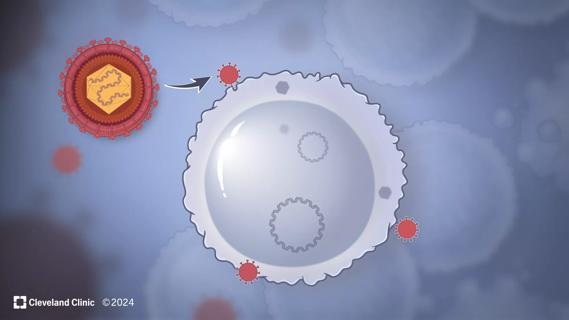
Cleveland Clinic researchers discover what drives – and what may halt – virus-induced cancer

Biologic approaches, growing implants and more
Previous studies, trial aims and the potential role of immunotherapy
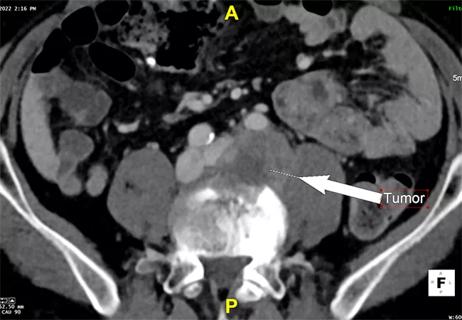
Invasion of the lumbar spine and iliac vein made resection risky