Invasion of the lumbar spine and iliac vein made resection risky
A 51-year-old male general surgeon presented to an out-of-state institution for progressive low back pain of two months’ duration. His past medical history was remarkable for testicular cancer treated 25 years earlier with orchiectomy and radiotherapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Imaging revealed a large mass invading the lumbar spine and left common iliac vein. Biopsy revealed it to be a spindle cell sarcoma, believed to be secondary to radiation changes following therapy for his testicular cancer. The patient came to Cleveland Clinic for evaluation.
The images in Figures 1-3 illustrate the complexity of potential management. Resection would risk damage to critical vasculature and require removal of a significant amount of spine.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c01b9133-ca84-41d2-b5e6-599010f0af2a/23-HVI-3529770-CQD-650x450-Inset1_jpg)
Figure 1. While the patient’s 3D CT on the left shows a normal-appearing aorta and iliac vein segment, the axial view on the right reveals an apple-sized tumor (arrow) lifting up the left common iliac artery and displacing the left common iliac vein, with intimate involvement of the spine from the L3 to L5 vertebral bodies.
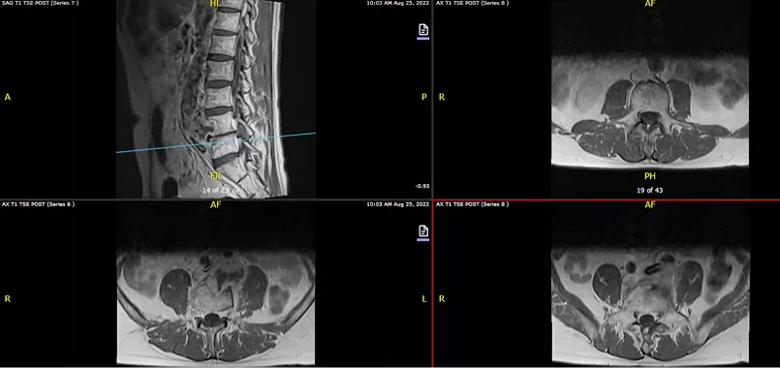
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2d24a2f3-256e-4a30-9287-de84037ab1ac/23-HVI-3529770-CQD-650x450-Inset2_jpg)
Figure 2. Sagittal and axial T1 MRI revealing a retroperitoneal mass invading the L4 vertebral body, abutting the L3 and L5 vertebral bodies and displacing the common iliac artery and vein.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f13a21d9-c535-4e34-81b7-10e360f8071c/23-HVI-3529770-CQD-650x450-Inset3_jpg)
Figure 3. Sagittal reconstructed and axial CT angiography again showing bony invasion of the L4 vertebral body and displacement of the left iliac artery and vein.
A course of neoadjuvant chemotherapy with doxorubicin and ifosfamide was initially pursued at the patient’s local institution under guidance from Cleveland Clinic oncologists. The tumor showed modest progression after two cycles of treatment, which prompted multidisciplinary exploration of the feasibility of tumor resection.
Spine surgery staff consulted with multidisciplinary colleagues — among others, surgical oncology and vascular surgery, in view of the vascular involvement — to discuss treatment possibilities. Together with the patient, they decided to proceed with short-course preoperative radiation therapy followed by a two-stage surgical plan to first stabilize the patient’s posterior spine and then to resect the tumor, reconstruct the venous system and further stabilize the spine from the front.
Advertisement
The first stage (Figures 4 and 5) was conducted by a team led by Center for Spine Health neurosurgeon Ajit Krishnaney, MD. Over nine hours, they performed T11-pelvis posterior instrumentation with iliac and S2 alar-iliac screw placement along with the following:

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/64565627-20a4-4b45-b5ce-9ccc625afbd0/23-HVI-3529770-CQD-650x450-Inset4_jpg)
Figure 4. Photos showing progressive steps in the first-stage operation. Left: Initial spine exposure. Middle: The spine after removal of posterior elements and screw placement. Right: Final construct.
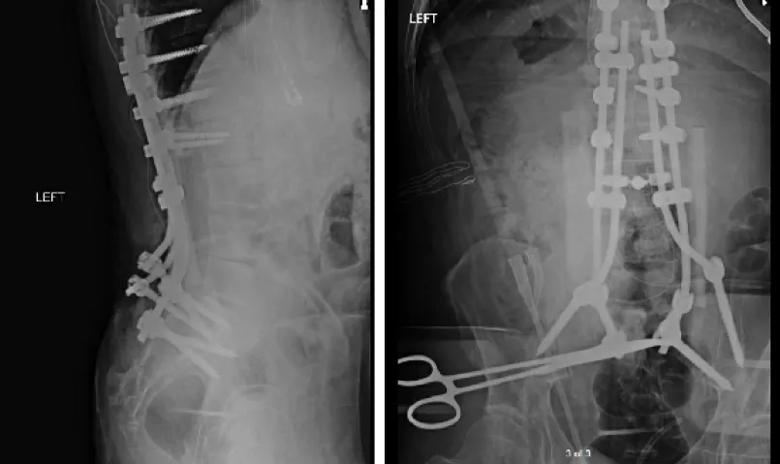
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/52a8bf2d-e581-4c88-8515-299ffb36d7c7/23-HVI-3529770-CQD-650x450-Inset5_jpg)
Figure 5. Intraoperative X-rays at the end of the first-stage operation showing the T11-pelvis construct with bilateral fibular allograft “boats” from L2 to the sacrum to allow for placement of local bone autograft and allograft posterolaterally.
Two days later, a multidisciplinary surgical team led by vascular surgeon Sean Lyden, MD, surgical oncologist Daniel Joyce, MBBCh, and Dr. Krishnaney resected the tumor (Figure 6) using an anterior approach. In addition to removal of the tumor, the 14-hour operation involved the following:
Advertisement
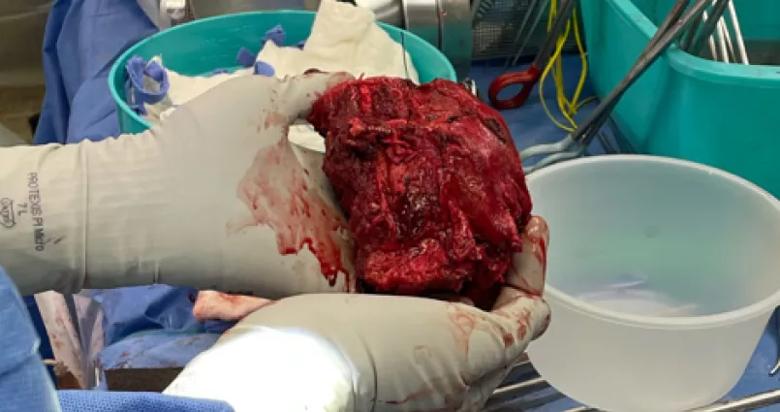
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f3e58914-27a2-452f-a3ac-75e1d32f127f/23-HVI-3529770-CQD-650x450-Inset6_jpg)
Figure 6. Photo of the resected specimen, which included the tumor, the iliac vein and vertebral bodies L3-5.
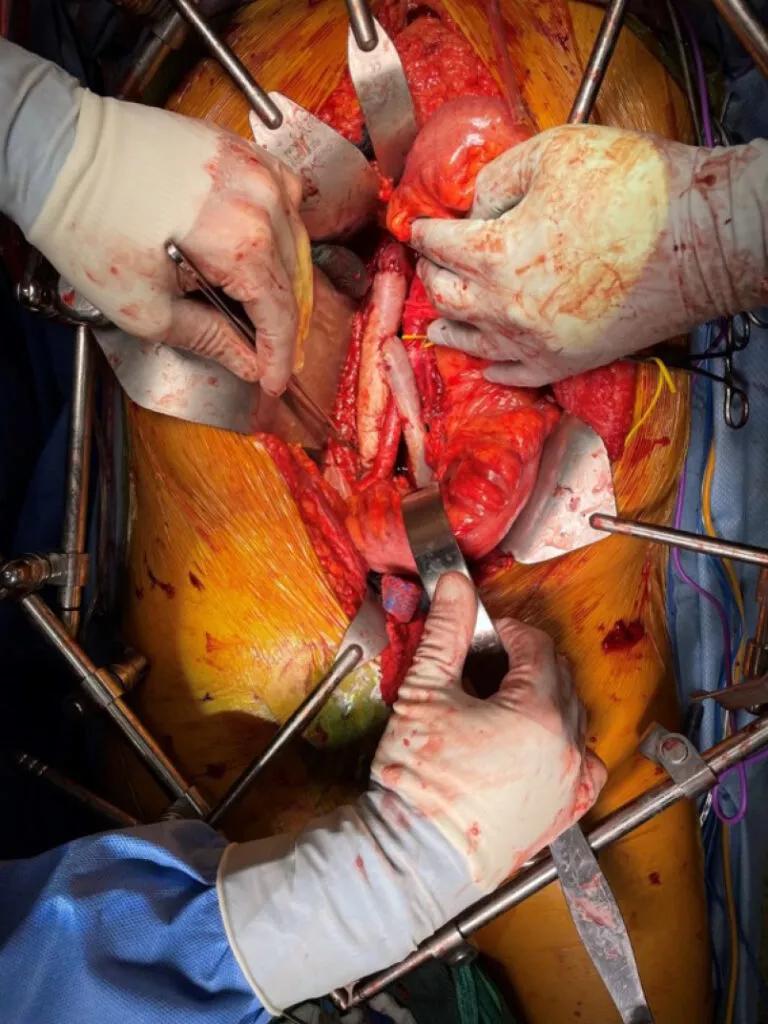
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7b77afcd-9407-4e08-add7-3446e401ebed/23-HVI-3529770-CQD-650x450-Inset7-768x1024_jpg)
Figure 7. Operative photo showing the reconstructed IVC.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9558cbb7-4ab4-4187-99a3-93cdd3fed495/23-HVI-3529770-CQD-650x450-Inset8_jpg)
Figure 8. Postoperative standing X-rays showing the final spinal reconstruction.
The patient fared well postoperatively. Despite the highly challenging tumor location, the team achieved a margin-negative (microscopic/R0) resection. It was decided to follow a course of active surveillance since the patient had received preoperative chemotherapy and radiation. He maintained his ability to walk safely despite removal of the three vertebral bodies, and there was minimal leg swelling. Imaging at three-month follow-up showed no recurrence of malignancy.
From vascular surgery. Dr. Lyden, who led the vascular surgery aspects of the operation, says this case is notable for at least three reasons. First is the daunting challenges the resection posed and the multispecialty collaboration required to overcome them. “An extremely limited number of U.S. institutions would have taken on this surgery and been able to pull off the interdisciplinary coordination required by this case,” he says. “This tumor would be deemed unresectable by virtually everyone, with vascular surgeons citing the spine involvement and spine surgeons citing the veins involved.”
Another point of distinction was the sheer size of the tumor in this location. “Resecting this tumor required removing all the bone from a 6-inch segment in the middle of the patient’s body,” Dr. Lyden notes. “The fact that our spine surgery colleagues could create enough spinal stability that the patient is able to walk is simply remarkable.”
Advertisement
The case is also notable for the ingenuity it required on the vascular surgery front. “There is not an off-the-shelf graft that could be used to reconstruct the vasculature we had to remove,” Dr. Lyden says, “so we took a sheet of bovine pericardium that’s used to patch arteries and we formed two long tubes to serve as the graft that was needed. When you practice at an institution like Cleveland Clinic where you’re immersed in innovation, fashioning solutions like this comes fairly naturally.”
From oncology. “This was an incredibly challenging case from an oncologic and technical standpoint,” says Dr. Joyce, who led the surgical oncology aspects. “It involved a high-grade radiation-induced sarcoma. We initially pursued a course of neoadjuvant, and unfortunately the tumor progressed slightly after two cycles of treatment. This obviously was a concerning feature with regard to the tumor biology.”
“Our initial oncologic instinct was to consider second-line chemotherapy,” Dr. Joyce explains, “but knowing the response rates, we were concerned that any further progression would lead to a truly unresectable tumor from a technical standpoint.” Moreover, he adds, the patient had significant toxicity from chemotherapy and was reluctant to consider further chemotherapy.
“We had an extensive discussion at our sarcoma tumor board and decided to proceed with preoperative short-course radiation,” he says. “One of the most important parts of this case was involving the patient and his family in decision-making, since the stakes were so high.”
Advertisement
From spine surgery. “This case was extremely challenging for a number of reasons, chiefly the size and location of the tumor and the number of critical structures in close proximity,” says Dr. Krishnaney, who led the spine surgery aspects. “When I first saw the patient, he had already been seen at a number of other large medical centers and been told the tumor was unresectable and he should proceed with chemotherapy and radiation. Being a physician, he understood his best chance of survival was if an oncologic resection could be performed.”
“At our first visit I thought it would be possible to resect the spinal portion of the tumor, but I was unsure whether the ventral portion could be safely accessed, resected and reconstructed,” Dr. Krishaney continues. “We presented the case at the multidisciplinary sarcoma tumor board, where experts from surgical oncology, vascular surgery, orthopaedics, medical oncology, radiation oncology, radiology and pathology could all discuss the case together and create a treatment plan. The interdisciplinary collaborative culture at Cleveland Clinic was critical to our ability to undertake and successfully complete this surgery. Having world-class physicians and surgeons from all these specialties in one place with the same goal is unusual in healthcare today. It’s what afforded us the opportunity to even attempt to resect this tumor.”
Advertisement
Personalized reconstruction is an alternative to leg amputation or flail limb
Soft tissue pathologist discusses research into incorporating genomic data to improve risk stratification
Machine learning models assess intraoperative tissue perfusion
For kids with painful, growing lesions in the arm, leg or pelvis
Cleveland Clinic researchers discover what drives – and what may halt – virus-induced cancer
Biologic approaches, growing implants and more
Previous studies, trial aims and the potential role of immunotherapy
Innovative construct restores function after resection of softball-size chondrosarcoma