ANA titers may by more dynamic than previously accepted
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Risk factors for developing subclinical autoimmunity and predictors for progression to clinical autoimmune phenotypes are poorly understood. An important step is to understand trajectories of antinuclear antibody (ANA) positivity and titers within individuals over time, and factors associated with these changes.
As part of the Gary S. Gilkeson Career Development Award from the Lupus Foundation of America, we performed an exploratory analysis of electronic health record (EHR) data to assess intraindividual variation in ANAs longitudinally. This work is in conjunction with Kelly Speth, MS, and Liu Wang, PhD, and Emily Somers, PhD, ScM, of the University of Michigan, and Jinoos Yazdany, MD, MPH, of the University of California, San Francisco.
Utilizing our academic health center’s EHR with records from 1999 through present, we extracted ANA (by immunofluorescence, IFA) and basic demographic data for all patients with at least one ANA. We also extracted ANA data for a subset of patients with validated systemic lupus erythematosus (SLE) by Systemic Lupus Erythematosus International Collaborating Clinics or American College of Rheumatology criteria. A titer of ≥ 1:80 was considered positive and a titer of < 1:80 was considered negative. We investigated the overall trend in ANA titer between each patient’s first and last observation by summarizing the number (and percentage) of SLE and control patients with a titer decrease, titer increase or stable titer. We evaluated changes in ANA titer over time using a baseline category logit mixed model with a patient-level random intercept where a separate fixed parameter for time was obtained for each comparison of a non-negative titer relative to a negative titer. We then estimated the odds of having a decreased titer value relative to a stable/increased titer at the next successive draw for various covariates using a generalized linear model.
Advertisement
A total of 6,546 unique patients had at least two valid ANA-IFA results. A subset of 52 of these patients had validated SLE, the remaining were considered controls. The majority of total patients were female (85%) and not Hispanic (90%) with a median age of 50 years. The mean number of valid ANA titers per patient was 2.6 (SD = 1.4), with a range of 2 to 20.
| Controls | SLE | Total | |
|---|---|---|---|
| Titer increase | 2,181 (33%) | 11 (21%) | 2,192 (33%) |
| No change | 2,129 (33%) | 23 (44%) | 2,152 (33%) |
| Titer decrease | 2,184 (35%) | 18 (35%) | 2,202 (34%) |
| Total | 6,494 | 52 | 6,546 |
| Titer increase | |||
| Controls | |||
| 2,181 (33%) | |||
| SLE | |||
| 11 (21%) | |||
| Total | |||
| 2,192 (33%) | |||
| No change | |||
| Controls | |||
| 2,129 (33%) | |||
| SLE | |||
| 23 (44%) | |||
| Total | |||
| 2,152 (33%) | |||
| Titer decrease | |||
| Controls | |||
| 2,184 (35%) | |||
| SLE | |||
| 18 (35%) | |||
| Total | |||
| 2,202 (34%) | |||
| Total | |||
| Controls | |||
| 6,494 | |||
| SLE | |||
| 52 | |||
| Total | |||
| 6,546 |
Longitudinally, ANA titer strength varied (p < 0.001). With the exception of a higher average odds of having a positive titer with each successive year [OR 1.84 (95% CI 1.62, 2.09)], no clear pattern of change between titers was identified (Figure 1). However, when evaluating the outcome of having a titer decrease (versus stable/increase) at the next successive observation, 32% of successive ANA draws had a decreased titer relative to the preceding titer. Among persons who were ANA-positive at baseline, 1,118 (22%) of the control subjects and two (4%) of the SLE subjects subsequently had a negative ANA. Among the SLE cases, titers decreased in 29% of successive draws (Fig 2). Controlling for basic demographic characteristics, being male increased the odds of having a decreased titer at the next successive draw (OR: 1.24, 95% CI: 1.11 – 1.40). Each successive year between ANA titers increases the odds of having a decreased titer (OR: 1.02, 95% CI: 1.01-1.04).
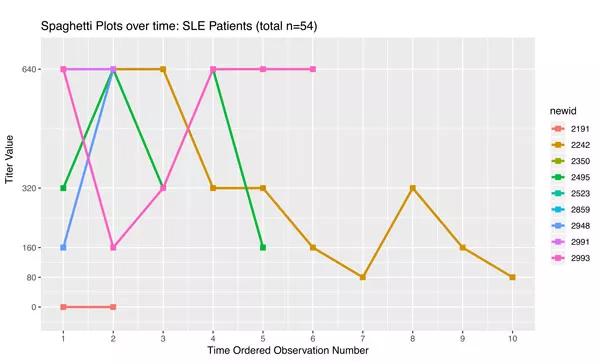
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dbec5606-df6a-4851-8073-e45b013893b1/spaghettiPlots-SLE_jpg)
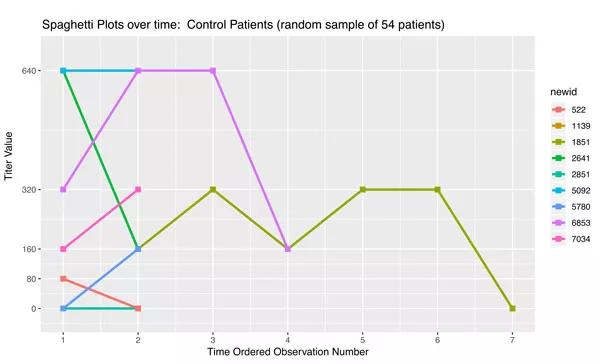
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2a02505d-241e-462e-961b-c529918d1442/spaghettiPlots-Control_jpg)
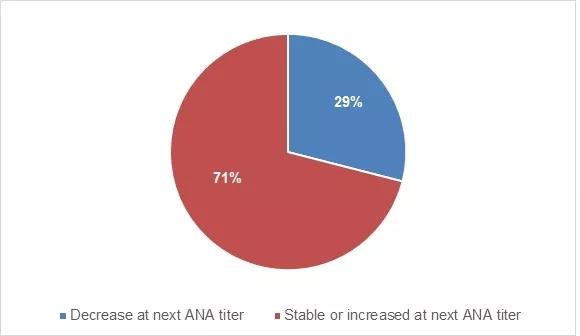
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/75397861-6bbb-40ca-8c39-fc4cd861ad5a/figure-2-1_jpg)
Although prior series of cross-sectional data suggest that ANAs tend to increase with age, longitudinal data of intra-individual patterns are lacking. Our data provide initial evidence of intra-individual variability. What is most novel about our findings is the downward trend of successive ANA titers, and their variability over time. Common clinical perception is that in SLE ANAs remain positive once antibodies are accrued, and that repeat testing would not influence management or alter diagnosis. Our data suggest that ANA titers may be more dynamic than previously accepted. We plan to investigate demographic and other covariates to further discern titers in different clinical phenotypes over time.
Advertisement
Advertisement

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.

Unraveling the TNFA receptor 2/dendritic cell axis