Case study evokes broad spectrum of clinical presentations that can be caused by underlying lupus
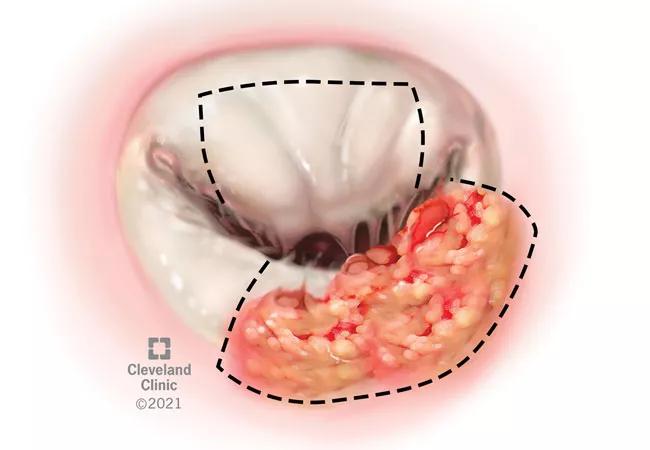
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d84c437d-f6be-40b7-ad7a-43b7a5fc5ee6/21-RHE-2059686-Littlejohn_Lupus-W-Libman-Sacks-EndocarditisAndAPS-CQD_650x450_jpg)
21-RHE-2059686-Littlejohn_Lupus-W-Libman-Sacks-EndocarditisAndAPS-CQD_650x450
After experiencing a cardiac event, a 38-year-old female was found to have left anterior descending coronary artery thrombosis requiring thrombectomy, stent placement and, eventually, coronary artery bypass grafting. Echocardiogram revealed mitral valve regurgitation and mitral valve vegetation. Following mitral valve replacement with left ventricular mass removal, results of laboratory studies were consistent with Libman-Sacks or marantic endocarditis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Libman-Sacks endocarditis is a nonbacterial thrombotic endocarditis secondary to inflammation, and the most common cardiac manifestation of systemic lupus erythematosus (SLE). Shortly after surgery, the patient’s antiphospholipid antibodies were found to be elevated, prompting referral to rheumatology. A review of her history revealed Raynaud’s phenomenon and migratory arthralgia, and her bloodwork showed an ANA titer of 1:320, elevated double-stranded DNA antibodies and lymphopenia as well as elevated creatinine. How would you proceed with diagnosis and treatment?
Watch Emily Littlejohn, DO, MPH, Director of the Cleveland Clinic Lupus Cohort (CCLC) and co-director of the Lupus Clinic, discuss the case in the video below. “It is my hope that this [case] will bring awareness to the broad spectrum of clinical presentations that can be caused by underlying lupus.”
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/K13gmcBJuoY?feature=oembed)
Lupus With Libman-Sacks Endocarditis and APS
In antiphospholipid syndrome (APS), antiphospholipid antibodies cause abnormal blood flow, which can lead to clotting in arteries and veins. It affects women more than men and is typically diagnosed between the ages of 30 and 40. Although antiphospholipid antibodies are present in about 40% of patients with SLE, only about half of those patients will develop thrombosis.
“This case illustrates the many faces of lupus with varying physical exam findings,” says Dr. Littlejohn. “Lupus can present in a myriad of ways. As rheumatologists, we need to have a keen eye to the many clinical presentations that may be atypical manifestations of systemic lupus erythematosus.”
Advertisement
Advertisement
Researching the biological basis for why treatment is or is not effective
Scribing system helps create more face-to-face interactions
A conversation with Leonard Calabrese, DO
The case for continued vigilance, counseling and antivirals
High fevers, diffuse rashes pointed to an unexpected diagnosis
No-cost learning and CME credit are part of this webcast series
Summit broadens understanding of new therapies and disease management
Program empowers users with PsA to take charge of their mental well being