This rare disease usually manifests as a firm, painless mass that is growing
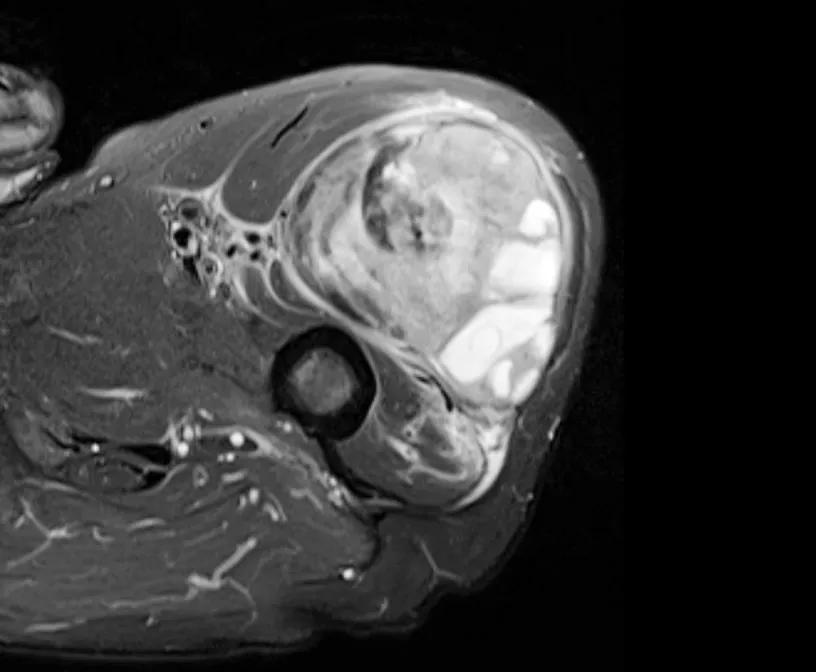
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/36ef9258-6597-4d74-8401-2a51e6f5577c/soft-tissue-sarcoma-MRI)
MRI of soft tissue sarcoma
Soft tissue sarcoma affects approximately 12,000-13,000 people in the U.S. each year. It is a type of sarcoma that occurs in muscle, fat, cartilage, ligaments, tendons, blood vessels, nerves and other connective tissues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Depending on how you interpret the molecular data, there are 50-100 subtypes of soft tissue sarcoma,” says Lukas Nystrom, MD, a Cleveland Clinic orthopaedic surgeon who specializes in musculoskeletal oncology.
Patients typically notice a growing mass, usually bigger than a golf ball, that is deep or just under the skin. Most often, it is painless.
“Patients typically seek us out after they notice the mass on their own or have some preliminary testing by their primary care physician that identifies a concern,” Dr. Nystrom says. “They come to our sarcoma team either to establish a diagnosis or get a second opinion. Really, we can meet them anywhere along their journey.”
Dr. Nystrom explained more about the diagnosis and treatment of soft tissue sarcoma in an episode of Cleveland Clinic’s Cancer Advances podcast.
Not all patients with a mass need to see a sarcoma specialist. Often, primary care physicians can determine if a mass is a subcutaneous lipoma — indicated as uniformly soft, small (golf-ball size) and right under the skin. Anything other than that should be imaged with an ultrasound and/or MRI scan. If concern arises following those tests, the case should be reviewed by a sarcoma specialist.
“When in doubt, refer,” Dr. Nystrom says. “The first step is getting an MRI or CT scan to better assess the mass. Those tests can indicate whether we are dealing with a lipoma or something more concerning. Definitive diagnosis requires a biopsy.”
Most soft tissue sarcomas can be diagnosed with a needle biopsy, preferably via a track that contaminates minimal tissue on the way to the tumor and that can be excised during a resection.
Advertisement
“We want to carefully orient that biopsy track with the potential surgical incision,” Dr. Nystrom says. “So, if there’s concern that a mass is sarcoma, I would rather perform the biopsy myself than have a patient come in with a biopsy in the wrong spot. That may lead to an increased risk of tumor recurrence.”
Following diagnosis of soft tissue sarcoma, Cleveland Clinic patients are evaluated by a multidisciplinary team including an orthopaedic or surgical oncologist, radiation oncologist, and medical oncologist. As an orthopaedic oncologist, Dr. Nystrom considers whether or not the patient is a candidate for limb-salvage surgery.
“The most important thing is to remove the tumor completely,” he says. “A wide surgical resection with negative margins while saving the limb is the ideal situation. But sometimes that is not possible, and the limb needs to be amputated to have a chance at eradicating the disease.”
Fifty years ago, soft tissue sarcoma was treated primarily with amputation. Since the development and refinement of MRI, it has become easier for surgeons to understand the extent of a tumor and, thus, more safely remove the tumor without amputation. Dr. Nystrom refers to an MRI scan as his “map” for a surgical resection.
Advances in radiation oncology have helped as well, allowing surgeons to leave narrower margins to save a nerve, blood vessel or bone, for example.
“One common misconception is that sarcoma in a limb means amputation,” Dr. Nystrom says. “It doesn’t. Today, we can save the limb most of the time. However, limb sarcoma surgery is not a minimally invasive procedure. Often, the required treatment compromises limb function, even though the limb still can be used.”
Advertisement
Radiation is often combined with surgery to decrease the risk of tumor recurrence. At Cleveland Clinic, all cases are discussed at a multidisciplinary tumor board that meets weekly to reach a consensus on treatment plans.
Cleveland Clinic physician researchers are making great strides in radiation therapy, trying to minimize its effects on healthy tissue near the tumor site. These effects, such as fibrosis that compromises joint function, can be limited with brachytherapy, a localized treatment that more precisely confines the effect of radiation compared to external beam radiation.
“Brachytherapy involves a focused delivery of radiation through tubes placed in the wound at the time of surgery — positioning the radiation source exactly where we want it,” Dr. Nystrom says. “It can’t be used in all cases, but it is effective when we do use it. We have been happy to see how it helps preserve limb function without compromising cancer outcome.”
Cleveland Clinic also uses short-course radiation for certain patients. This approach condenses radiation therapy before surgery from five weeks to only one.
“It is effective in controlling the cancer, but we have been selective about who gets this treatment, so further work is necessary to understand this course better,” Dr. Nystrom says. “It is a major improvement in patient experience. If you can do it without compromising cancer control, it is a big win.”
Advertisement
Advertisement
Meta-analysis suggests efficacy and safety
Machine learning models assess intraoperative tissue perfusion
Approach could help clinicians identify patients at an increased risk of progression who could benefit from more aggressive treatment
A recent case study illustrates surgical intervention for treating recurrent bladder cancer
How it’s similar but different from the direct anterior approach
Collaboration must cross borders and disciplines
Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols
Should surgeons forgo posterior and lateral approaches?