How to manage cases from early symptoms to referral: A guide for PCPs
One of the challenges in treating soft tissue sarcoma (STS) is that patients often present with advanced disease at diagnosis. Therefore, recognizing symptoms and referring patients for treatment early in the course of illness is an important goal in securing an optimal clinical outcome.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Any time we’re dealing with a malignancy, it is logical that early detection and treatment are important, even though in the case of STS, studies have not been able to prove a better outcome with a specific time-to-diagnosis,” says Lukas Nystrom, MD, orthopaedic oncologist in Cleveland Clinic’s Department of Orthopaedic Surgery.
Any mass the size of a golf ball and growing should be suspected for sarcoma, Dr. Nystrom maintains. Since sarcomas are typically not painful, pain should not be used as a diagnostic criterion.
“Physicians and patients should look out for large, deep lumps that are increasing in size without any specific symptoms of systemic disease,” says Dr. Nystrom. “Lumps due to sarcoma can be anywhere – under the skin or deep in the muscle and are typically firm and painless.”
According to a recent study, patients older than 69 with symptoms lasting longer than 8-16 weeks and tumors greater than 10 cm that are increasing in size have a 94.7 percent likelihood of malignancy. Conversely, smaller tumor size is associated with an absence of metastases and better prognosis — it has been estimated that only about 3 percent of patients with a STS smaller than 5 cm in size have metastasis.
Dr. Nystrom adds that patients with certain types of cancer syndromes, such as Li-Fraumeni, and those who were exposed to radiation, may be at greater risk of developing STS. However, the vast majority of patients with STS have no identifiable risk factors.
Once STS is suspected, a range of imaging techniques are available for further evaluation.
Advertisement
“We often use ultrasound to examine a small mass underneath the skin,” says Dr. Nystrom. “In case of a deep or larger mass (golf ball sized, or larger), magnetic resonance imaging (MRI) of the affected region is recommended. MRI is a very sensitive technique, but can have false positives, as some conditions mimic sarcoma, most notably infections and hematomas.”
After initial imaging, a needle biopsy is performed to confirm the suspected STS diagnosis.
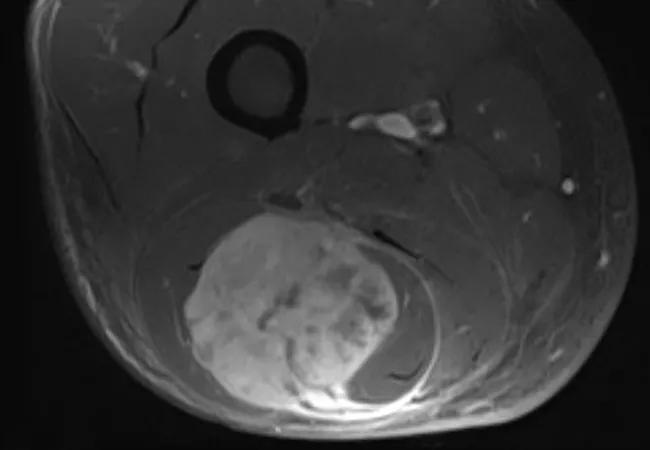
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0ff2aba3-19a6-4f93-86a2-0c53420b6785/18-ORT-1081-Nystrom-Hero-Image-650x450pxl_jpg)
Axial T1 post-contrast MRI of the thigh showing soft tissue sarcoma prior to resection.
“Primary care physicians should refer patients to a surgeon as soon as an MRI is suspicious for sarcoma and before the biopsy,” Dr. Nystrom cautions. This is very important because “a biopsy should be performed by the surgeon who will be doing the resection if it proves to be a STS. The biopsy track should ideally be excised with the surgical resection specimen and, therefore, this is best planned by the surgeon performing the operation.”
According to Dr. Nystrom, if the mass is located in the arms or legs, patients should be referred to an orthopedic oncologist. If it is located in the abdomen, patients should see a general surgeon (surgical oncologist).
“First-line therapy for STS is surgical resection, which is most often performed in combination with radiation therapy in case of deep and high-grade or aggressive tumors,” says Dr. Nystrom. “Chemotherapy may also be used depending on tumor type, grade and size.”
Patients who don’t have metastases and are treated with combination therapy have reason to be optimistic about their prognosis.
Advertisement
“While many variables come into play, nonmetastatic STS at the time of presentation, treated early, can be a curable disease,” Dr. Nystrom says, adding that multidisciplinary sarcoma teams are equipped to attain the best outcomes for such patients.
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment