Why multidisciplinary surgical and cancer teams are essential
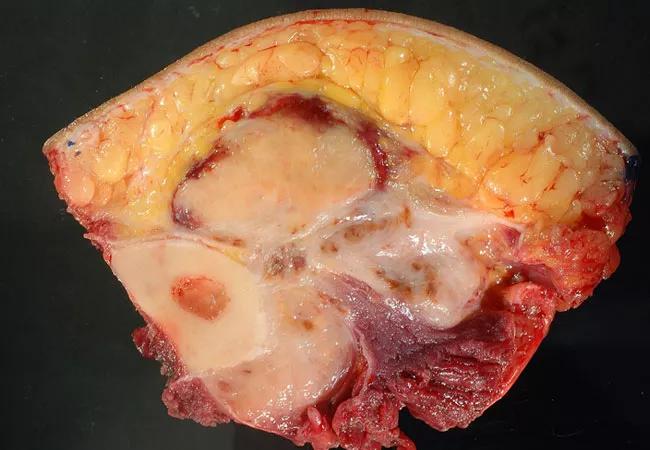
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/eb4c892d-cd6c-4b00-9056-f543db956a2f/20-ORI-1943011-CQD-Bridging-the-Gap-Hero_jpg)
20-ORI-1943011-CQD-Bridging-the-Gap-Hero
By Nathan Mesko, MD; Lukas Nystrom, MD; and Timothy Marks, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Diaphyseal bone tumors present unique challenges in reconstruction. Compared to malignant and benign bone tumors close to a joint, diaphyseal bone tumors occur at a rare incidence. Tumors typically found in the diaphysis of long bones can be found in Table 1. Tumor histology, patient age and comorbidity status, segment defect size, and patient prognosis all are important considerations to factor in when determining the appropriate type of reconstruction technique. Oftentimes, a multidisciplinary surgical team is required for reconstruction to address soft tissue coverage and re-vascularization concerns. Appropriate planning and a coordinated surgical effort are essential in leading to a successful outcome.
Table 1. Differential Diagnoses for Diaphyseal Bone Tumors (“AEIOU and Sometimes Y”)
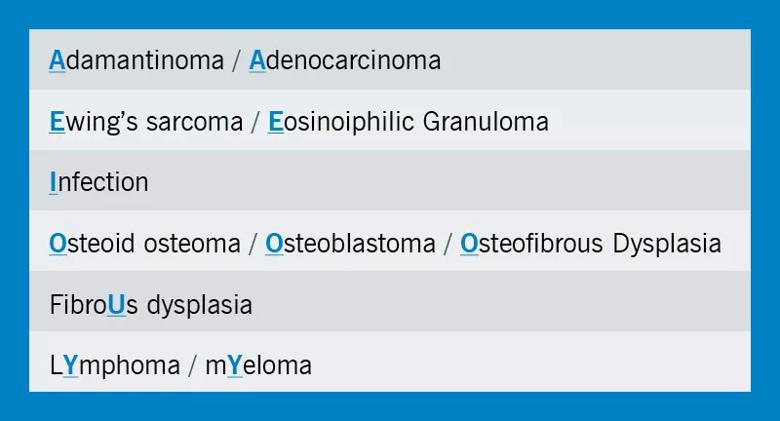
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/24d29a7e-318c-4866-8f30-3a506e499604/20-ORI-1943011-CQD-Bridging-the-Gap-Charts-1_jpg)
A 23-year-old former marine presented with one year of tibial pain that progressed to a point where he quit running. Imaging (Figure 1) suggested a diaphyseal tibial lesion. A core needle biopsy of the large lytic lesion (red arrow) suggested a classic type of adamantinoma. Systemic staging studies showed localized disease only.
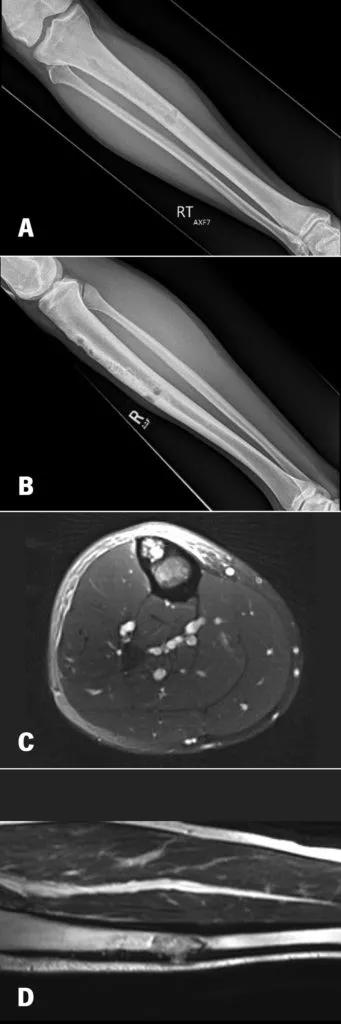
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7521f746-9188-4c5c-b564-e6603e1b3991/20-ORI-1943011-CQD-Bridging-the-Gap-Fig-1-341x1024_jpg)
Figure 1. 28-year-old with 12 months of tibial pain. AP and Lateral Radiographs (A, B) show a cortically based anterior tibial lesion, with axial (C) and coronal (D) MRI imaging suggesting cortical breakthrough and an aggressive marrow replacing process.
A 17 cm segmental resection was performed with a proximal metaphysis junctional step cut. A bulk tibial allograft was fashioned to mirror the segmental defect and the construct was dual plated. The plastic surgery team rotated a regional gastrocnemius flap over the diaphysis to aid with soft tissue coverage.
Advertisement
Eight months post-op, the patient began having pain at the distal junction site. X-rays revealed a broken lateral plate and multiple broken screws (Figure 2). The proximal junction had healed uneventfully. He underwent a second operation to exchange hardware and graft the junction site with iliac crest autograft. His distal junction has gone onto union six months post-op, and he is now four years out from his original tumor resection (Figure 3).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b26207a4-3f1c-4865-9c23-5311c7184a44/20-ORI-1943011-CQD-Bridging-the-Gap-Fig-2_jpg)
Figure 2. AP and Lateral (A, B) radiographs 8 months post-op of the right tibia, showing a healed proximal junction, but a nonunion at the distal diaphyseal junction with broken screws noted.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/db6ca3e6-df4e-473e-a72a-870f4daa552e/20-ORI-1943011-CQD-Bridging-the-Gap-Fig-3_jpg)
Figure 3. AP and Lateral (A, B) radiographs 6 months after the patient underwent nonunion surgery, with a plate revision and iliac crest bone grafting. The proximal and distal junctions have gone on to union, with no functional activity restriction.
A 46-year-old school administrator presented with an incidentally discovered distal tibial soft tissue mass, discovered during a routine primary care physician visit. Imaging suggested an aggressive appearing soft tissue mass adjacent to the posterior tibial vessels and partially encasing the tibial diaphysis (Figure 4), while CT staging studies suggested an isolated 9 mm pleural based mass. An image-guided biopsy revealed a high-grade dedifferentiated liposarcoma.
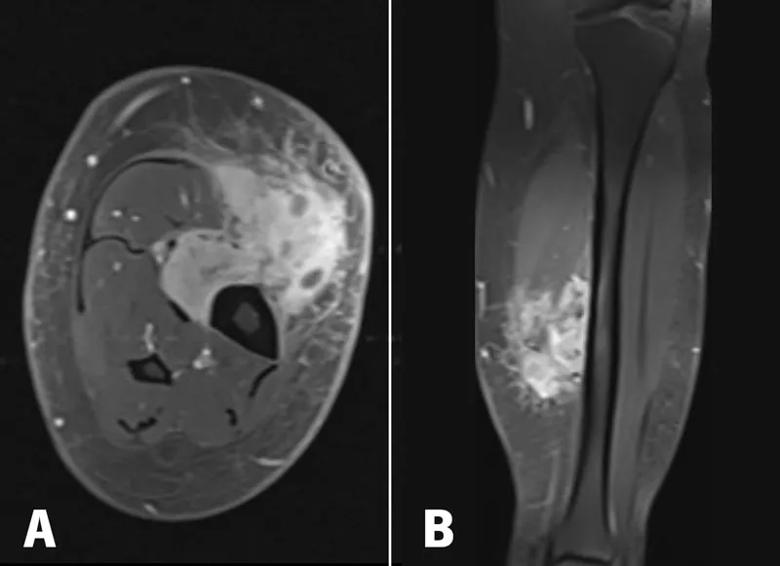
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1d839f01-254b-41bb-9c1a-b0c2165c5d1c/20-ORI-1943011-CQD-Bridging-the-Gap-Fig-4_jpg)
Figure 4. Post-contrast T1 axial (A) and coronal (B) MRI imaging shows a heterogenously enhancing mass involving the superficial and deep posterior compartments with invasion thru the investing calf fascia into the subcutaneous layer. The bone was surrounded by more than 180 degrees.
Advertisement
The patient underwent five weeks of preoperative radiotherapy. Re-staging studies suggested a stable pleural based mass. Multiple options for defect reconstruction were discussed, taking into account the patient’s morbid obesity and the large soft tissue defect that would require a free soft tissue flap transfer.
A coordinated multidisciplinary effort was completed between the orthopaedic oncology, plastic surgery and vascular surgery teams. A 9 cm intercalary tibial resection was made to facilitate a clean margin resection, along with sacrifice of the posterior tibial vessels (Figure 5). The tibial defect was then reconstructed with an intercalary endoprosthetic device with interlocking screws distal and proximal. A reverse saphenous vein graft bypass and a contralateral free tensor fascia latae flap was then performed for soft tissue coverage (Figure 6). He was made toe-touch weight-bearing for 12 weeks following surgery to allow for bony ingrowth of the prosthesis and soft tissue healing.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1e2339d3-9f43-43ce-8763-f017bc935512/20-ORI-1943011-CQD-Bridging-the-Gap-Fig-5_jpg)
Figure 5. Gross cross-section of the resection specimen, showing the tumor surrounding the bone and invading both sides of the investing calf fascia.
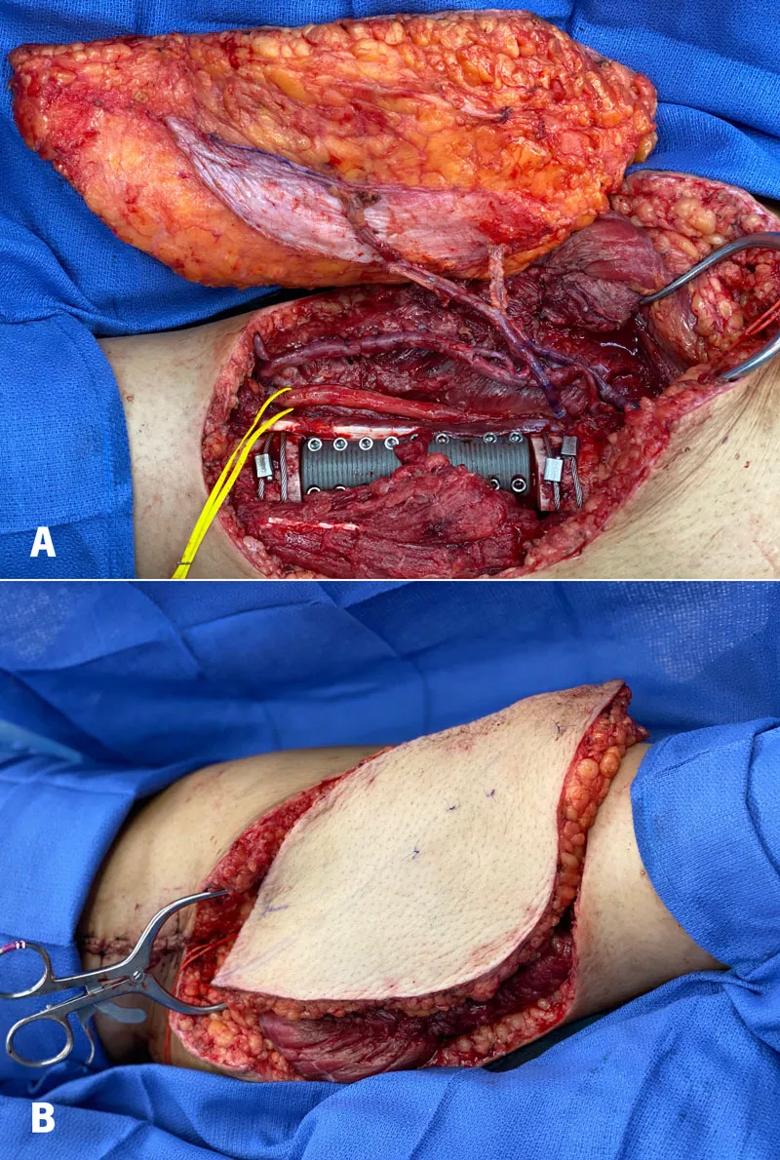
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0a032f31-b610-466b-b8b3-fdbf28bd196d/20-ORI-1943011-CQD-Bridging-the-Gap-Fig-6_jpg)
Figure 6. A contralateral leg ALT flap was harvested and sewn into the posterior tibial vessel reverse saphenous vein bypass graft, to restore inflow and outflow to the flap (A). The 9cm tibial defect was reconstructed using a pressfit intercalary tibial implant with interlocking screws proximal and distal. The final inset of the fasciocutaneous flap is pictured (B). Post-op radiographs are also noted (C).
Advertisement
In young patients, biologic solutions can be ideal. While these solutions are oftentimes more complex and can span a long timeline of healing, the biologic bridging of bone provides a lower long-term complication risk profile. Fibular Autograft, used by itself or to help supplement a bulk allograft, is one option. Bone Transport (Distraction osteogenesis) is another option that provides a biologic solution for an intercalary defect. This can be done with an external fixation device, over a transport intramedullary nail, or with a combination of a plate and nail construct (Plate-Assist Bone Transport, PABST) (Figure 7).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7c5c5ff7-bb55-498b-83b6-52b62c0feb15/20-ORI-1943011-CQD-Bridging-the-Gap-Fig-7-284x1024_jpg)
Figure 7. Distraction Osteogenesis, or Bone Transport, is an evolving technique that can use either external frame or a combination of plate/nail constructs, non-invasively lengthening over a magnetized intramedullary nail device. Figure A shows a diaphyseal Ewing Sarcoma with a skip metastasis that has undergone lengthening utilizing plate-assist-bone transport (PABST) to transport across a defect and “dock” at the distal junction (B-D).
Allograft is a standard option for defect reconstruction but comes with the potential for longer-term complications, such as allograft fracture, nonunion at the junction sites requiring re-grafting surgery, graft resorption, or infection. Likewise, an intercalary implant has potential loosening and infection complications, that may be solved with newer generation implants that allow for better fixation to the bone. Despite this, metal implants allow for more immediate weight-bearing and shorter intraoperative reconstruction times.
Advertisement
No one solution is perfect for every patient, and an informed decision based on the partnership of the multidisciplinary team and patient is vital in lending to success. Table 2 summarizes reconstruction techniques and their advantages/disadvantages.
Each patient diagnosis and scenario presents unique variables and qualities that require a multidisciplinary surgical and cancer team to work together in formulating a specific plan tailored to each patient. Walking the journey with our patients through their surgical and surveillance journey is our top priority, while also attempting to maintain maximum function with various reconstruction techniques.
Table 2. Summary of Diaphyseal Bone Reconstruction Techniques
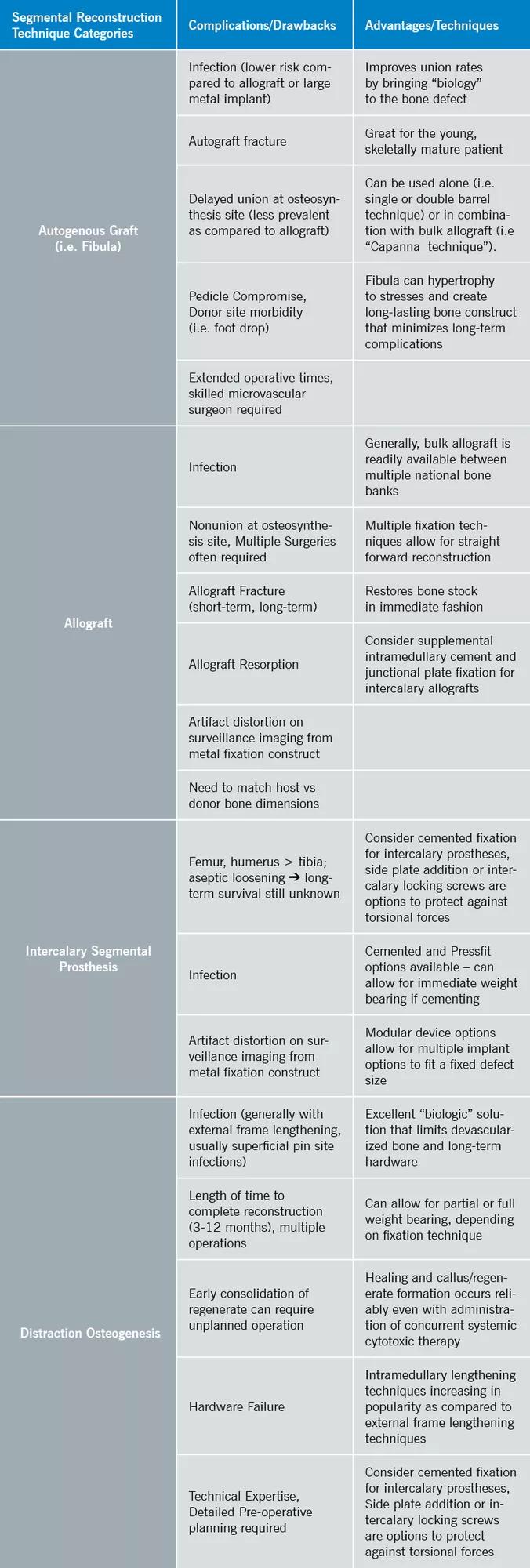
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6dffe549-7bbc-449d-afc7-fc14695711c9/20-ORI-1943011-CQD-Bridging-the-Gap-Charts-2_jpg)
Dr. Mesko is Director of the Musculoskeletal Tumor Center, and Co-Director of the Sarcoma Program at Cleveland Clinic; Dr. Nystrom is co-director of the Pediatric Sarcoma program and Vice Chairman of Quality for the Orthopaedic & Rheumatologic Institute; Dr. Marks is an orthopaedic oncologist with the Cleveland Clinic Akron General Orthopaedics Oncology team.
Advertisement
How it’s similar but different from the direct anterior approach
Collaboration must cross borders and disciplines
Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols
Should surgeons forgo posterior and lateral approaches?
How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians
Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes
Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction
Percutaneous stabilization can increase mobility without disrupting cancer treatment